Medical billing teams are under more pressure than ever. Insurance companies are denying more claims, documentation requirements keep getting more complicated, and the cost of mistakes keeps climbing. Each documentation error from an undertrained staff member triggers a claim denial that costs $25-50 to fix. Multiply that across thousands of claims monthly, and poor staff training directly wrecks your finances.
Medical billing training is how you equip your revenue cycle staff with everything they need to accurately document patient encounters, submit clean claims, manage denials, and stay compliant with regulations. Here’s the thing: 50% of providers say missing or inaccurate claim data is the top reason for denials. That makes proper training absolutely critical to your bottom line.
Certified billing professionals arrive with solid coding knowledge. They understand ICD-10, CPT, and HCPCS fundamentals. But certification doesn’t teach them how your practice management system works, what your top payers specifically require, or how your organization handles complex scenarios. New hires typically spend 30-90 days learning these organization-specific workflows through shadowing experienced staff and trial-and-error, an approach that leaves too much to chance when documentation accuracy directly affects revenue.
This guide walks you through a structured four-week approach to training medical billing teams using TextExpander. We’ll show you how combining solid training methods with smart Snippet libraries and collaborative documentation systems accelerates organizational knowledge transfer, cutting onboarding time dramatically while improving claim accuracy and reducing expensive billing errors.
Free: Medical Billing Snippets
Download 27 TextExpander Snippets to help make your medical billing team more accurate and more consistent. Save time and reduce denied claims.
The Complete Steps to Train New Medical Billing Team Members
Training new medical billing staff takes structure. You can’t just throw someone into a billing system and hope for the best. The process breaks down into eight steps that take new hires from their first day through independent work. Each step builds on the last one.
Step 1: Complete Pre-Training Requirements and Compliance Education
Before new staff touch patient information or billing systems, they need to complete compliance training and background checks. This usually happens in the two weeks before their official start date. When they show up on day one, they’re ready for actual training instead of spending their first week on paperwork.
Background checks verify that staff meet healthcare standards for working with protected health information. The process includes criminal background verification, reference checks from previous employers, and credential verification for relevant certifications. Services like Checkr, GoodHire, or Verified First complete these checks within 5-7 business days when applications come in promptly.
HIPAA training covers patient privacy rules, what happens if you violate them, how to handle protected health information properly, secure communication practices, and breach reporting procedures. Everyone working with patient data must complete HIPAA training before accessing systems with patient information—the HIPAA Privacy Rule (45 CFR §164.530) requires this. The Department of Health and Human Services offers free training resources, though many organizations use commercial platforms like HealthStream or Relias that provide certificates and track completion dates for audits.
Other compliance requirements vary by organization but often include OSHA safety training, fraud and abuse prevention covering the False Claims Act and Anti-Kickback Statute, sexual harassment prevention, and workplace violence prevention. These modules protect both the organization and individual staff members by setting clear behavioral expectations and legal obligations.
System access setup happens at the same time as compliance training. IT departments create user accounts in the practice management system, electronic health record, clearinghouse portal, payer authorization systems, and TextExpander for organizational knowledge access. Getting credentials before day one means new staff can log in right away when training starts, which beats waiting around for access requests to process.
Step 2: Build Foundation in Medical Terminology and Billing Concepts
Medical billing requires fluency in healthcare language. You can’t accurately process claims if you don’t understand what you’re reading. The goal here is building that foundational vocabulary—without it, more advanced training won’t stick.
Basic medical terminology covers body systems and anatomical terms, common diagnoses and their plain-language equivalents, standard procedures and treatments, medical abbreviations used in documentation, and specialty-specific vocabulary relevant to your organization. A cardiology practice needs deeper terminology around cardiovascular conditions than a general practice, while an oncology center requires extensive cancer staging and treatment vocabulary. Tailor terminology training to your actual service lines rather than generic healthcare vocabulary that staff will never encounter in daily work.
Understanding the revenue cycle shows how claims become revenue. Cover patient registration and insurance verification, charge capture and coding, claim submission, payment posting, denial management, patient statements and collections, and reporting and analytics. New staff need to see how their specific role fits into this broader process and how errors at any stage affect organizational revenue.
Insurance fundamentals distinguish between coverage types and their rules. Coverage includes commercial insurance from major carriers, Medicare Parts A, B, C, and D, Medicaid and managed Medicaid plans, workers’ compensation, and auto insurance for accident-related care. Each payer type has different rules for prior authorization requirements, documentation standards, timely filing limits, and appeal processes. Understanding these differences prevents claim submission errors that result in denials.
Medical coding basics introduce the classification systems used in billing. Start with ICD-10 diagnosis codes including structure, format, specificity requirements, and how to read code descriptions. Then CPT procedure codes including E/M levels, surgery codes, and modifier usage. Also HCPCS Level II codes for supplies, medications, and ambulance services. And the concept of medical necessity linking diagnoses to procedures. New staff don’t need deep coding expertise unless they’re specifically hired as coders, but everyone processing claims needs baseline coding literacy to recognize obvious errors or mismatches.
TextExpander snippet libraries help here—common diagnosis codes with plain language descriptions, frequently used CPT codes for standard procedures, modifier explanations and usage examples, insurance carrier contact information and requirements. New staff can reference these resources during training rather than memorizing everything upfront.
Step 3: Provide Hands-On Software Training with Your Specific Systems
Medical billing staff spend their days in specialized software. How well they know these tools directly determines productivity. The focus here is building proficiency with the actual systems your organization uses rather than generic software training that doesn’t match real workflows.
Practice management system training covers the backbone of billing operations. Trainees learn patient demographics and insurance entry, appointment scheduling and charge capture, claim generation and submission, payment posting and adjustment entry, aging reports and collections tools, and reporting capabilities for tracking performance metrics. Systems like Athenahealth, NextGen, AdvancedMD, or Kareo each have different interfaces and workflows, so training must be system-specific rather than conceptual.
Electronic health record integration shows how clinical documentation becomes billing data. Show trainees how providers document encounters, how charges flow from the EHR to billing system, how to review documentation for billing accuracy, identifying missing or incomplete documentation, and when to query providers for clarification. Organizations using integrated systems like Epic or Cerner need to teach how clinical and financial systems communicate, while those with separate systems need to show how data transfers between platforms.
Clearinghouse portal navigation covers claim scrubbing and submission. Clearinghouses like Change Healthcare, Waystar, or Availity act as intermediaries between provider systems and payers, performing real-time claim validation before submission. Trainees learn claim submission workflows, how to interpret scrubbing reports and error messages, making corrections before claims reach payers, tracking claim status through the clearinghouse, and downloading remittance advice and payment files.
Payer portals provide direct access to insurance carrier systems for eligibility verification and getting prior authorizations online, checking claim status, starting appeals and reconsiderations, and downloading explanation of benefits and fee schedules. Staff working with your top insurance carriers need portal credentials and training on each payer’s specific system since interfaces vary dramatically between United Healthcare, Aetna, Blue Cross, and Medicare.
Create sandbox training environments whenever possible where new staff can practice without affecting live data. Most major practice management systems support training databases that mirror production environments but don’t submit actual claims or affect patient records. Trainees can make mistakes safely while building the muscle memory that translates to production confidence.
Step 4: Conduct Role-Specific Training for Your Billing Positions
Medical billing departments have distinct roles with different responsibilities and skill requirements. Training needs to be customized to each position type rather than giving identical training regardless of job function.
Patient access specialists focus on front-end revenue cycle functions including insurance verification and eligibility checking, getting prior authorizations, collecting copayments and deductibles at time of service, scheduling appointments, and communicating financial policies to patients. These staff need strong customer service skills and knowledge of payer-specific requirements but don’t require deep coding expertise. Training emphasizes communication, problem-solving with insurance companies, and financial counseling conversations.
Medical coders translate clinical documentation into billing codes. This specialized role requires extensive training in anatomy, medical terminology, disease processes, ICD-10 diagnosis coding with 70,000+ possible codes, CPT procedure coding with thousands of codes and modifiers, HCPCS coding for supplies and medications, coding guidelines and compliance requirements, and auditing for accuracy and compliance. Most organizations require professional certification from AAPC (Certified Professional Coder) or AHIMA (Certified Coding Specialist) for coding positions, representing 6-12 months of dedicated study and examination. Training programs for coders extend well beyond general billing staff timelines.
Claims processors handle the technical aspects of claim submission including entering charges into the billing system, validating codes and modifiers, scrubbing claims before submission, correcting claim errors, tracking claim status through clearinghouses and payer portals, and resubmitting corrected claims. These positions require strong attention to detail, understanding of claim formats and requirements, and familiarity with common rejection reasons. Training focuses on system navigation, error interpretation, and correction workflows.
Denial management specialists work specifically on appealed or denied claims including analyzing denial reasons and patterns, researching payer policies and coverage decisions, preparing appeal letters with supporting documentation, tracking appeal deadlines and resubmission requirements, and communicating with providers about documentation needs. This advanced role requires deep knowledge of payer policies, strong writing skills, clinical understanding, and persistence. Training includes studying common denial codes, appeal writing, and regulatory requirements.
Payment posters handle incoming remittances including posting insurance payments and contractual adjustments, posting patient payments, identifying and resolving underpayments, transferring balances between insurance and patient responsibility, and reconciling daily deposits. Training emphasizes explanation of benefits interpretation, payment posting accuracy, and identifying posting errors that affect accounts receivable aging.
Role-specific snippet libraries make sense here. Patient access specialists get verification scripts and financial policy explanations. Coders get diagnosis and procedure code templates with documentation requirements. Denial specialists get appeal letter templates organized by denial reason. Each position gets exactly the resources they need.
Step 5: Build Competency Through Realistic Practice Scenarios
Conceptual knowledge doesn’t mean much if staff can’t apply it to actual billing situations. Now it’s time to transition from passive learning to active problem-solving using scenarios that mirror the challenges staff will face in production work.
Create practice exercises based on your actual service mix. An orthopedic practice should use fracture care, joint injections, and surgical cases rather than generic examples. A mental health practice needs scenarios involving psychotherapy codes, substance abuse treatment, and psychiatric medication management. Realistic scenarios help staff recognize the specific patterns they’ll encounter rather than memorizing theoretical examples they’ll never use.
Use anonymized denied claims as learning exercises. Real denials provide authentic examples of coding errors, documentation deficiencies, medical necessity issues, and technical claim problems. Walking through why claims were denied and how to correct them builds pattern recognition faster than manufactured examples. Maintain a library of de-identified denied claims categorized by denial reason to use as training materials for new staff.
Structure scenarios with progressive complexity. Start with straightforward single-diagnosis, single-procedure encounters where coding and billing are obvious. Progress to encounters with multiple diagnoses requiring proper sequencing, multiple procedures requiring modifier selection, coordination of benefits between multiple payers, and payer-specific requirements that differ from standard billing practices. This graduated approach builds confidence through early success while steadily increasing difficulty.
Include role-play exercises for patient-facing positions. Practice difficult conversations like explaining large patient balances, requesting payment from financially stressed patients, clarifying coverage limitations, and responding to complaints about billing problems. These rehearsals build confidence for emotionally challenging situations that new staff often find intimidating.
Give immediate feedback on practice scenarios rather than waiting until training completion to identify problems. When trainees make errors, explain why the approach was incorrect and demonstrate the right method. Immediate correction prevents bad habits from forming and speeds up learning by connecting action to outcome.
Scenario libraries with common billing situations, expected responses, and correction templates let new staff work through exercises independently. They can check their responses against documented solutions, allowing self-paced learning that supplements instructor-led training.
Step 6: Shadow Experienced Staff During Live Billing Work
Theoretical knowledge and practice scenarios provide foundation, but watching skilled billers handle real-world complexity demonstrates expertise that training materials can’t fully capture. Pair new staff with experienced team members to observe expert decision-making and problem-solving in action.
Structure shadowing in 2-3 week rotations covering different workflow stages and staff specialties. New hires should shadow patient access during registration, experienced coders during documentation review, claims processors during submission workflows, denial specialists during appeal preparation, and payment posters during remittance processing. This comprehensive exposure shows how work flows through the revenue cycle and how different roles interact.
Encourage mentors to talk through their thought process while working. The most valuable learning happens when experienced staff explain why they make specific choices, what red flags they watch for, how they prioritize competing tasks, and when they seek help versus solving problems independently. This running commentary transforms observation into active learning.
Let trainees ask questions freely during shadowing without worrying about interrupting workflow. The goal is learning, not maximum productivity during these rotations. Experienced staff should expect questions and view teaching as part of their role during these periods.
Transition gradually from observation to supervised practice. After watching a workflow several times, trainees can attempt tasks while the mentor observes and provides real-time coaching. This supported practice builds confidence before independent work.
Document mentor knowledge through snippets capturing standard approaches to common problems, decision trees for complex situations, and troubleshooting guides for frequent errors. This institutional knowledge transfer benefits both trainees and creates organizational assets that outlast individual staff tenure.
Step 7: Implement Gradual Independence with Quality Reviews
Moving from supervised practice to independent work requires careful monitoring to catch errors before they become patterns. What you need now is a progressive quality review system that maintains oversight while gradually increasing autonomy as competency improves.
Start with 100% review of all work products during the first weeks of independent billing. Every claim, every payment posting, every verification should be checked by an experienced staff member before finalizing. This intensive oversight catches errors immediately, provides frequent correction opportunities, and prevents problematic claims from reaching payers.
Reduce review frequency as accuracy improves. Move from 100% review to 50% review, then 25% review, then 10% spot-check review as trainees demonstrate consistent accuracy. Track error rates to guide review reduction decisions rather than following arbitrary timelines. A trainee consistently achieving 95%+ accuracy can reduce review frequency faster than someone with persistent errors.
Use structured error logs documenting every mistake including the error type, root cause, whether it was a knowledge gap or careless mistake, the correction made, and any pattern with previous errors. These logs identify specific areas requiring additional training and show whether mistakes reflect systematic misunderstandings or random oversights requiring different intervention approaches.
Conduct weekly one-on-one meetings during the independence phase covering error patterns from quality reviews, areas of improvement and remaining development needs, questions about processes or policies, productivity metrics compared to expectations, and timeline to full independence. These regular touchpoints maintain support while giving trainees clear feedback about their progress.
Quality assurance snippets help here—common error patterns, correction procedures, and documentation templates. Both trainees and reviewers can use standardized audit forms ensuring consistent evaluation criteria regardless of which experienced team member conducts the review.
Step 8: Establish Continuous Education and Advanced Competency Development
Training doesn’t end when staff achieve independence. You need systems for ongoing learning that keep teams current with industry changes and develop advanced capabilities that increase value over time.
Annual coding updates require regular training. The Centers for Medicare & Medicaid Services updates ICD-10 codes each October, while the American Medical Association releases new CPT codes each January. HCPCS codes update quarterly. Teams need training sessions covering new, deleted, and revised codes relevant to your specialty, guideline changes affecting documentation requirements, payer policy updates related to the code changes, and practice management system updates required to support new codes.
Monitor payer policy changes that affect billing practices. Insurance companies frequently modify coverage policies, prior authorization requirements, documentation standards, and payment methodologies. Establish processes for reviewing payer newsletters and bulletins, testing billing changes before implementation, updating internal procedures to match new requirements, and communicating changes to affected staff. Missing policy updates results in denied claims and revenue loss.
Conduct regular denial trend analysis to identify learning opportunities. Monthly reviews should examine denial rates by category and payer, patterns suggesting process or knowledge gaps, new denial reasons requiring investigation, and opportunities for preventive education. When denials cluster around specific issues, implement targeted training to address root causes rather than repeatedly correcting the same errors.
Encourage cross-training across billing functions so staff understand adjacent roles and can provide backup coverage during absences. Coders benefit from understanding denial management. Payment posters gain insight from watching patient access interactions. This broader perspective improves collaboration and problem-solving while building organizational resilience.
Support professional certification and continuing education for career development. Many billing professionals pursue credentials from AAPC, AHIMA, or the Healthcare Financial Management Association. Organizations investing in certification preparation, exam fees, and continuing education units demonstrate commitment to staff development that improves retention while building organizational expertise.
Keep living documentation of policy updates, code changes, and process modifications through regularly updated snippet libraries. When policies change, update the relevant snippets so everyone accesses current information rather than outdated procedures. This keeps institutional knowledge current without manual procedure manual updates.
Understanding the financial impact of documentation errors
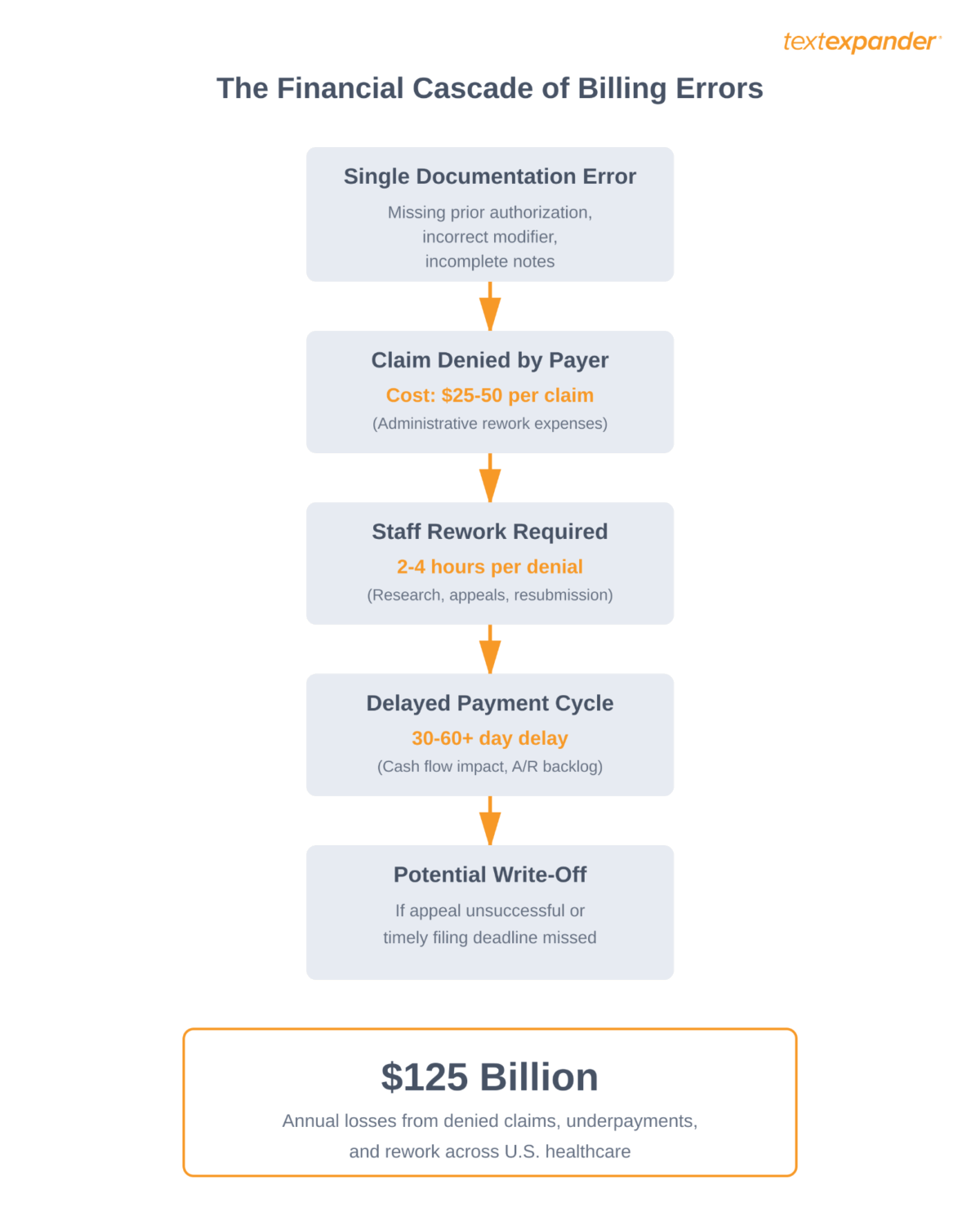
Documentation failures in medical billing cost a staggering amount of money. Healthcare systems waste an estimated $125 billion annually through denied claims, underpayments, and administrative rework. That’s real revenue that should have been captured through proper billing practices.
The math is brutal. When a claim gets denied because of missing information, wrong codes, or documentation that doesn’t support the billed service level, you have to spend more resources to appeal or resubmit. Studies show each denied claim costs between $25 and $50 to rework. Process thousands of claims monthly? Those costs add up fast.
Beyond direct rework costs, bad training creates problems throughout the revenue cycle. Staff who lack proper training take longer to process claims, creating bottlenecks that delay cash flow. They miss payer-specific requirements, triggering automatic denials that could have been prevented. They don’t catch documentation gaps before submitting claims, pushing problems downstream instead of catching them early.
Healthcare organizations operate on slim profit margins, so documentation accuracy isn’t just a quality metric: it’s about survival. When documentation failures cost millions annually, the organizations that invest in better training systems gain a real competitive advantage.
How training gaps lead to claim denials
The connection between poor training and claim denials is direct and measurable. When you analyze denial patterns, you’ll find that most denials come from preventable errors: missing information, wrong patient demographics, coding that doesn’t match documentation, or failure to get required authorizations.
The 2025 Experian Health State of Claims Report shows that 50% of providers identified missing or inaccurate claim data as the primary cause of denials in 2025, up from 46% in 2024. The report also reveals that 41% of providers now experience denial rates of 10% or higher, a continuing upward trend since 2022.
Here are the billing errors that come from poor training: missing or incorrect patient demographic information causes immediate rejections at the clearinghouse level, incorrect modifier usage signals improper billing for the service level provided, failure to verify insurance eligibility before service results in claims submitted to inactive policies, incomplete documentation doesn’t support the billed service level and triggers medical necessity denials, duplicate billing for services already processed indicates lack of understanding of claim status workflows, and incorrect place of service codes violate payer contracts or Medicare rules.
Each of these errors represents a knowledge gap that proper training should fix. When new billing staff get inadequate training, they pick up incorrect processes or develop workarounds that seem efficient but violate payer requirements. These bad habits become hard to correct once they’re established.
The problem gets worse because each insurance company has unique requirements. What Medicare accepts, commercial payers might deny. What Blue Cross processes smoothly, Aetna might reject for lack of prior authorization. New billing staff have to learn not just general principles but the specific quirks and requirements of dozens of payers.
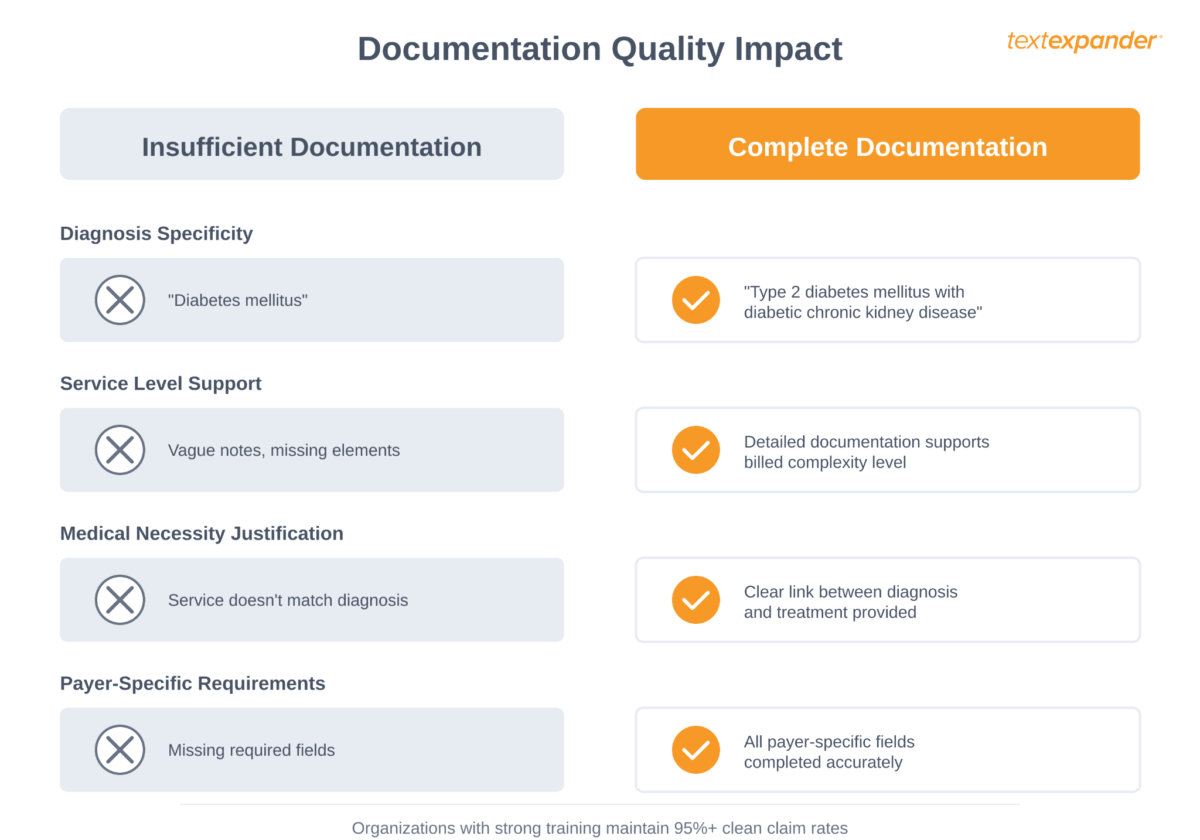
Organizations with solid training systems see measurably better outcomes. They maintain clean claim rates above 95%, meaning fewer than one in twenty claims needs rework. They process claims faster because staff catch errors before submission. Most importantly, they capture revenue that organizations with weaker training systems leave on the table.
Week one: Organization-specific documentation workflows
The first week of training establishes how your organization applies documentation standards in practice. Instead of overwhelming new staff with every possible scenario, week one focuses on translating their certification knowledge into your specific systems, workflows, and requirements.
Essential documentation standards
Medical billing operates on standardized code sets that provide a common language across the healthcare industry. New staff need to understand three primary code systems: ICD-10-CM for diagnoses, CPT for procedures and services, and HCPCS for supplies and specialized services.
ICD-10-CM (International Classification of Diseases, 10th Revision, Clinical Modification) codes describe patient diagnoses and symptoms. These codes tell the payer why the patient needed care. Proper training emphasizes the importance of specificity. “Diabetes mellitus” isn’t sufficient when the documentation supports “Type 2 diabetes mellitus with diabetic chronic kidney disease.” The more specific the diagnosis code, the better it supports medical necessity for the services provided. Later, we’ll demonstrate how TextExpander can help there.
CPT (Current Procedural Terminology) codes describe what was done for the patient. These codes range from basic office visits to complex surgical procedures. New billing staff have to learn to match documentation to the appropriate service level. An evaluation and management code for a comprehensive visit with high medical decision-making requires substantially more documentation than a brief, straightforward encounter.
HCPCS (Healthcare Common Procedure Coding System) codes cover supplies, equipment, and services not included in CPT. These codes become particularly important for practices that provide durable medical equipment, certain drugs, or specialized services.
The foundation week should include hands-on practice with real documentation examples. Staff should practice identifying the appropriate codes based on provider notes, recognizing when documentation is insufficient to support a particular code level, and understanding how diagnosis codes must support the medical necessity of procedure codes.
Certified billing professionals already understand these code sets from their training. The challenge in week one isn’t teaching codes but teaching how your organization applies them. Which diagnosis codes do your top providers typically use? How does your documentation support different E&M levels in your EHR? What are your organization’s internal coding policies that differ from textbook guidelines? This organizational context is what transforms textbook knowledge into productive work.
What certification teaches vs. what organizations must train
Certified billing professionals arrive with valuable foundational knowledge: they understand medical terminology, know how to use code books, grasp basic compliance requirements, and can navigate standard billing concepts. This education typically takes 4-12 months and costs thousands of dollars.
What they don’t arrive knowing: how your specific practice management system is configured, which fields your organization tracks that others don’t, what your top ten payers’ unique requirements are, how your organization sequences diagnosis codes for specific scenarios, which services trigger extra scrutiny from your payer mix, where your EHR stores the information they need, and what your internal escalation procedures are for complex situations.
This organizational knowledge gap typically takes 30-90 days to fill through shadowing, questions to experienced staff, and learning from mistakes. TextExpander helps close this gap faster through systematic knowledge capture in Snippet libraries.
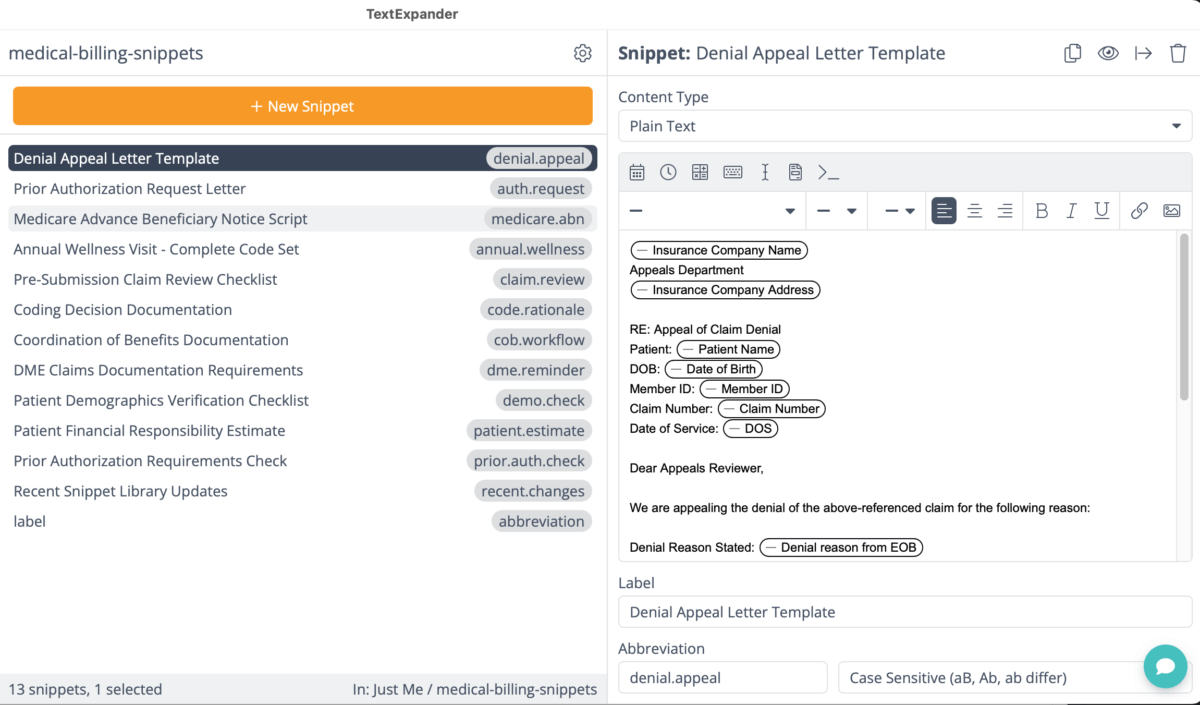
Creating your first TextExpander Snippet library
Here’s where TextExpander changes the game: instead of expecting new staff to learn your organization’s specific requirements through osmosis, you capture that knowledge in Snippet libraries. A certified biller knows what a prior authorization is, but your Snippet library teaches them exactly how YOUR organization handles prior auth requests for YOUR top payers, in the specific formats THEY require, using YOUR internal tracking system.
TextExpander changes how you approach documentation training by letting you capture institutional knowledge in reusable Snippet libraries. Instead of expecting new staff to memorize hundreds of organization-specific requirements, payer quirks, and internal processes, Snippets make expert knowledge instantly available.
Start by creating a core library of essential Snippets that new billing staff will use daily. These should include frequently used diagnosis and procedure code combinations for your organization’s most common encounters. For example, a primary care practice might create a Snippet that expands “annual.wellness” into the complete set of codes for an annual wellness visit, including appropriate diagnosis codes, the wellness visit CPT code, and any commonly-billed preventive services.
Standard responses to common payer requests also belong in the core library. When a payer requests additional documentation, staff can use pre-approved response Snippets rather than writing responses from scratch. This ensures consistency and compliance while saving time. A Snippet might expand “auth.request” into a complete prior authorization request letter with all required elements in the format that particular payer demands.
Patient demographic verification checklists ensure staff collect all required information before submitting claims. A Snippet could expand “demo.check” into a formatted checklist that verifies patient name spelling, confirms date of birth, validates insurance ID number, checks subscriber relationship, verifies insurance is active, and confirms prior authorization if required.
Compliance reminders for services that require special handling protect against common mistakes. For high-risk services that frequently trigger denials, create Snippets that remind staff of requirements. For example, “dme.reminder” might expand into a checklist of documentation elements required for durable medical equipment claims.
The power of Snippet libraries becomes clear when organizational requirements change. When a major payer updates its prior authorization requirements, you update one Snippet rather than retraining every team member. When new regulations affect documentation standards, you modify the relevant Snippets and the knowledge automatically spreads to everyone’s workflow.
During week one, new staff should learn to access and use these pre-built Snippets, understand how Snippets reduce errors by ensuring consistent documentation, and begin recognizing situations where Snippets would be valuable in their daily work.
Hands-on practice with real scenarios
Theory means nothing without application. Week one should include structured practice sessions using realistic scenarios based on your organization’s actual billing patterns.
Create practice exercises that mirror common encounters. Provide new staff with provider documentation and have them identify the appropriate codes, determine if documentation is sufficient, identify potential issues that might cause denials, and use TextExpander Snippets to prepare the claim for submission.
These practice sessions reveal knowledge gaps before they cause real-world claim denials. When a trainee selects an incorrect code during practice, you can immediately correct the misunderstanding. When they miss a required field, you can reinforce why that information matters for claim success.
Practice scenarios should get progressively more complex. Early exercises might involve straightforward office visits with clear documentation. As the week progresses, introduce scenarios with ambiguous documentation that requires clarification, multiple diagnoses that must be sequenced correctly, services that require prior authorization, or payer-specific requirements that differ from standard practices.
The goal isn’t perfection by the end of week one but rather building a solid foundation of core knowledge and establishing good habits. Staff should leave week one understanding how code sets work together, recognizing common documentation patterns, comfortable using Snippet libraries for standard tasks, and aware of how their role affects organizational revenue.
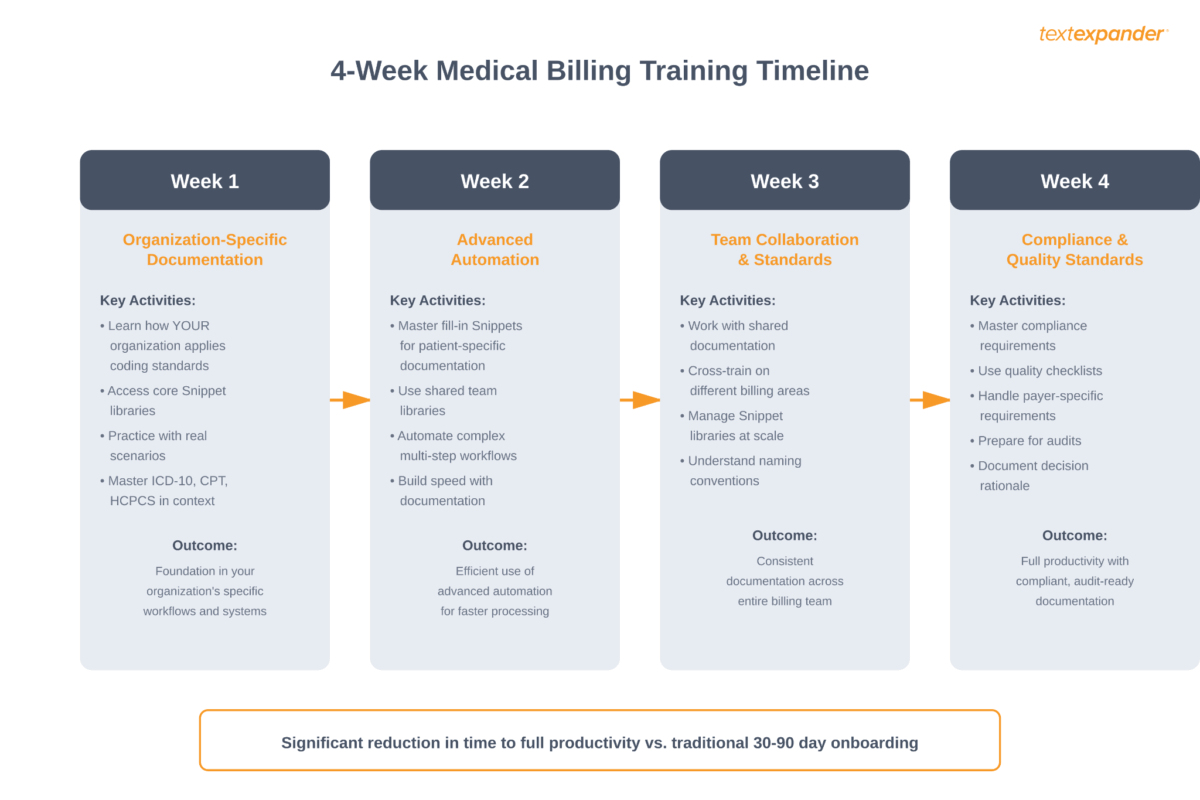
Week two: Leveraging TextExpander’s advanced features
Week two builds on the foundation by introducing advanced automation features that dramatically speed up billing workflows. By the end of this week, staff should be using TextExpander not just for basic code insertion but for managing complex, multi-step processes.
Dynamic fill-in Snippets for patient-specific documentation
Fill-in Snippets turn static text into intelligent templates that prompt for patient-specific information. These Snippets create consistency while maintaining the flexibility needed for individualized documentation.
A fill-in Snippet for denial appeal letters might prompt for patient name, date of service, claim number, specific denial reason, and supporting documentation references. Staff complete these prompts, and TextExpander generates a complete, professionally formatted appeal letter that includes all required elements in the payer’s preferred format.
This feature proves particularly valuable for documentation that follows standard structures but requires patient-specific details. Instead of starting from a blank document or copying and pasting from previous examples (which risks errors when details aren’t fully updated), staff use fill-in Snippets that ensure nothing gets overlooked.
Common applications for fill-in Snippets in medical billing include prior authorization request letters that require patient demographics, provider information, diagnosis justification, and service details. The Snippet prompts for variable information while auto-filling standard elements like provider credentials and office contact information.
Payer-specific claim notes that must follow particular formats benefit from fill-in Snippets. Some payers require claim attachments in specific structures. Fill-in Snippets ensure staff include all required sections while customizing content for the individual claim.
Patient financial responsibility estimates that calculate costs based on deductibles, copays, and coinsurance work well as fill-in Snippets. The Snippet prompts for the relevant financial variables and generates a complete, accurate estimate in a standard format that patients can easily understand.
Coordination of benefits documentation when patients have multiple insurance policies becomes manageable through fill-in Snippets. The Snippet walks staff through the complex process of determining primary and secondary payer responsibility, ensuring they follow correct claim submission sequences.
Shared team libraries for consistent documentation
Shared Snippet libraries ensure every team member works from the same playbook. When organizational best practices, payer requirements, or regulatory guidelines live in shared libraries, knowledge doesn’t stay siloed with experienced staff members.
Create specialized libraries organized by function. A “Prior Authorization” library contains all Snippets related to authorization processes. A “Denial Management” library includes appeal templates, common denial responses, and escalation procedures. An “Insurance Verification” library provides scripts for calling payers and checklists for confirming coverage details.
The collaborative nature of shared libraries means documentation improves continuously. When a billing specialist discovers a more effective way to phrase a particular type of appeal, they update the Snippet. That improvement immediately becomes available to everyone. When a supervisor identifies a common error pattern, they modify the relevant Snippet to prevent future occurrences.
Shared libraries also make quality control easier. Supervisors can review and approve Snippets before they enter the shared library, ensuring all documentation meets organizational standards. This approval workflow prevents well-intentioned but incorrect information from spreading through the team.
Week two training should include instruction on accessing different shared libraries, using library search functions to quickly find needed Snippets, understanding the organization’s approval process for Snippet modifications, and contributing improvements to shared libraries when staff identify opportunities.
Automating complex workflows with fill-in Snippets
Advanced TextExpander users create comprehensive Snippets with multiple fill-in fields that guide staff through entire workflows, not just individual documentation tasks. These structured Snippets reduce the mental load on billing staff while ensuring consistent execution of complex processes.
Think about the complete workflow for submitting a claim that requires prior authorization. The process involves verifying patient coverage, determining if the service requires authorization for that specific payer, submitting the authorization request with appropriate clinical documentation, tracking the authorization request status, updating patient records with the authorization number, and only then submitting the actual claim.
A well-designed fill-in Snippet can guide staff through each step with prompts. The Snippet includes fill-in fields that ask: Does this payer require authorization for this service? What’s the patient information? What’s the clinical justification? The expanded Snippet then generates the complete authorization request in the payer’s required format, creates a tracking entry, and includes a reminder about follow-up timing.
This approach is particularly valuable for processes that happen infrequently enough that staff don’t memorize every step but frequently enough that they can’t afford errors. Authorization requests for specialty medications, appeals of denied claims at various levels, coordination of benefits for patients with multiple insurance policies, and credentialing documentation for new providers all benefit from structured fill-in Snippets.
Week two should include training on recognizing opportunities for workflow automation, designing effective fill-in field sequences, testing and refining complex Snippets for your organization’s specific processes, and documenting these Snippets so others can understand and use them effectively.
Measuring efficiency gains
By the end of week two, staff start seeing measurable improvements in their efficiency. Beyond simply typing faster, TextExpander eliminates repetitive typing entirely through intelligent Snippet expansion. Billing specialists using well-developed automation tools can expect to process claims significantly faster than those relying on manual entry and reference materials.
Track specific metrics during week two to demonstrate progress. Measure time required to complete common tasks like processing a standard office visit claim, preparing a prior authorization request, or responding to a payer documentation request. Compare these times to organizational benchmarks or to the trainee’s own performance earlier in training.
Document error rates during practice exercises. As staff become comfortable with Snippets and automation, their error rates drop noticeably. A trainee who made five mistakes per ten practice claims in week one should be making two or fewer by the end of week two.
These measurable improvements build confidence and reinforce the value of the training approach. When staff see concrete evidence that they’re getting faster and more accurate, they engage more fully with the training process and tell their colleagues about these tools.
See how TextExpander works in healthcare →
Week three: Enhancing team collaboration with TextExpander
Week three shifts focus from individual efficiency to team coordination. Medical billing succeeds or fails based on how well team members share information, maintain consistency, and support each other through complex cases.
Building a culture of shared knowledge
The most effective billing teams treat documentation knowledge as a shared resource rather than individual expertise. TextExpander’s collaborative features support this cultural shift by making it easy for team members to contribute to and benefit from collective knowledge.
Encourage staff to contribute Snippet improvements when they discover more effective approaches. If a team member finds that a particular phrasing increases appeal success rates with a specific payer, they should update the shared Snippet so everyone benefits. When someone identifies a common error pattern, they should create or modify Snippets to prevent that error.
This collaborative approach requires clear protocols. Designate Snippet library managers responsible for reviewing and approving contributions. Create a submission process for new Snippets or modifications. Schedule regular review sessions where the team discusses Snippet library updates and shares insights about what’s working well.
Recognition reinforces contribution. When a team member’s Snippet improvement leads to better outcomes, acknowledge their contribution in team meetings. When someone creates a particularly valuable new Snippet, share that success with leadership. These acknowledgments encourage ongoing participation in building shared knowledge.
Standardizing responses to common scenarios
Consistency in billing communication matters. When different team members respond to the same type of payer inquiry with different information or formatting, it creates confusion and potentially raises red flags that trigger additional scrutiny.
Shared Snippet libraries enable perfect consistency for standard communications. All prior authorization requests follow the same structure and include the same essential elements. All level-one appeal letters use the same opening language and follow the same argumentative structure. All patient financial responsibility estimates present information in identical formats.
This consistency doesn’t mean robotic inflexibility. Fill-in Snippets maintain the standardization that builds trust with payers while allowing appropriate customization for individual circumstances. The structure stays constant while the specific details change to reflect each unique situation.
Focus week three training on identifying scenarios that require standardized responses, developing or refining Snippets for these scenarios, practicing using standard responses while incorporating case-specific details, and understanding when and how to deviate from standard templates for exceptional cases.
Cross-training through shared documentation
Shared Snippet libraries make cross-training easier by making expertise transferable. When an experienced denial management specialist’s knowledge exists as documented Snippets, other team members can handle denial management tasks in her absence.
This cross-training capability is crucial for maintaining revenue cycle continuity. Medical billing teams struggle when key staff members take vacation or leave the organization. If one person “owns” all knowledge about Medicare appeals or prior authorization for specialty medications, their absence creates bottlenecks.
Snippet libraries distribute this knowledge. The processes and language that the expert uses become available to everyone. While less experienced staff might work more slowly, they can complete the task correctly because the expert’s approach is captured in usable format.
Week three should include exercises where team members work outside their primary specialization using shared Snippet libraries. The claims submission specialist should practice denial appeals using the denial management library. The authorization specialist should process standard claims using the claims submission library. These cross-training exercises reveal gaps in documentation and help staff appreciate the full scope of the revenue cycle.
Managing Snippet libraries at scale
As organizations build extensive Snippet libraries, organization and maintenance become critical challenges. Week three training should address the practical aspects of managing hundreds or thousands of Snippets.
Teach staff effective naming conventions that make Snippets easy to find. Abbreviations should be intuitive and follow consistent patterns. For example, all Medicare-related Snippets might begin with “mc,” all authorization Snippets with “auth,” and all appeal Snippets with “app.” This consistency makes Snippets discoverable even when users don’t remember exact abbreviations.
Set up a regular review schedule for Snippet libraries. Healthcare billing requirements change constantly. Medicare updates its policies quarterly. Commercial payers modify authorization requirements unpredictably. Shared Snippet libraries have to stay current with these changes.
Designate team members as subject matter experts for particular libraries. One person takes responsibility for keeping the Medicare Snippets current. Another maintains the prior authorization library. These designated experts monitor for regulatory changes, payer policy updates, and internal process improvements that require Snippet modifications.
Week three should wrap up with staff understanding how Snippet libraries are organized in your organization, knowing who to contact with questions about specific libraries, being able to find needed Snippets quickly even in extensive libraries, and understanding the process for requesting updates or additions to shared libraries.
Week four: Ensuring compliance and quality standards
The final week of foundational training addresses the critical connection between documentation accuracy and regulatory compliance. Medical billing operates within a complex regulatory framework, and documentation failures can trigger audits, recoupments, and even fraud investigations.
Understanding compliance requirements in medical billing
Compliance in medical billing covers adherence to federal healthcare regulations, Medicare and Medicaid policies, commercial payer contract requirements, HIPAA privacy and security rules, and professional ethical standards.
New billing staff have to understand that compliance isn’t optional or negotiable but rather the foundation of sustainable revenue cycle operations. Organizations that develop reputations for billing errors face increased scrutiny from payers, more frequent audits, and difficulty contracting with insurance networks.
Key compliance concepts for week four include medical necessity, which requires that all services billed must be medically appropriate for the patient’s condition and documented by the treating provider. Claims submitted without proper medical necessity documentation face denial and potential recoupment if paid initially.
Correct coding principles require using the most specific code that accurately describes the diagnosis or service. Upcoding (billing for a more complex service than was provided) and unbundling (separately billing components of a service that should be billed together) are considered fraudulent practices that can result in severe penalties.
Documentation must support the level of service billed. Billing for a comprehensive examination requires documentation of a comprehensive examination. The provider’s notes must explicitly support every element of the billed service. This principle, summarized as “if it wasn’t documented, it wasn’t done,” protects both the provider and the organization.
HIPAA compliance governs all handling of patient information. Billing staff must understand permitted uses and disclosures of protected health information, security requirements for electronic systems, minimum necessary standards for accessing patient data, and breach notification requirements if security incidents occur.
Creating documentation quality checklists
Quality control in medical billing relies on systematic review before claim submission. TextExpander Snippets can embed quality checklists directly into billing workflows, ensuring staff verify critical elements before claims go out the door.
A comprehensive claim review checklist verifies that patient demographics match insurance records exactly, diagnosis codes support medical necessity for all services billed, procedure codes accurately describe services documented by provider, modifiers are used correctly and only when required, prior authorization numbers are included for services requiring authorization, diagnosis codes are sequenced correctly with primary diagnosis first, all required fields are complete with no missing information, and the claim follows any payer-specific formatting or documentation requirements.
Instead of expecting staff to remember every item on this checklist, create a TextExpander Snippet that expands the entire checklist into the claim notes field or into a separate verification document. Staff work through the checklist systematically, confirming each element before submission.
For high-risk claim types that frequently trigger audits or denials, create enhanced checklists with additional verification steps. Claims for expensive specialty medications might include extra checks on diagnosis specificity and medical necessity documentation. Claims for evaluation and management services at high complexity levels might require detailed verification that documentation supports the level billed.
Week four training should emphasize that these checklists aren’t bureaucratic obstacles but rather protection for the organization and the individual staff member. When a claim later faces audit or review, systematic checklist completion provides documentation that due diligence was performed.
Audit preparedness through consistent documentation
Organizations face audits from various sources including Medicare Recovery Audit Contractors, commercial payer audit programs, Office of Inspector General investigations, and internal compliance reviews. Consistent documentation practices through TextExpander Snippets create defensible audit trails.
When auditors request documentation, they’re looking for evidence that claims were supported by appropriate documentation, billing followed payer rules and regulations, any errors were promptly identified and corrected, and the organization has systems in place to prevent improper billing.
Snippet-based documentation helps address these audit concerns. Because Snippets ensure consistent processes, auditors see evidence of systematic approaches rather than random practices. Because Snippet libraries incorporate compliance requirements, documentation automatically includes elements that auditors expect to find. Because shared libraries enable review and approval, there’s clear evidence of oversight and quality control.
Train staff to document their decision-making process using Snippets. When a billing decision requires judgment (for example, selecting between two potentially appropriate codes), the staff member should document why they chose a particular code. A Snippet might expand “code.rationale” into a formatted note explaining the coding decision with reference to the supporting documentation.
This documentation of reasoning protects the organization during audits. Even if an auditor disagrees with a coding decision, clear documentation of the reasoning behind the decision shows good faith effort and systematic decision-making rather than careless or fraudulent billing.
Handling payer-specific requirements
One of the toughest aspects of medical billing is managing the unique requirements of dozens of different insurance payers. What Medicare requires differs from what Blue Cross Blue Shield requires, which differs from what Aetna requires. These requirements change regularly, sometimes without warning.
TextExpander Snippets provide a solution for managing payer-specific complexity. Instead of expecting staff to memorize each payer’s unique requirements, create payer-specific Snippet libraries that encode these requirements into usable workflows.
A Medicare-specific library might include Snippets for Medicare’s Advance Beneficiary Notice requirements, Medicare Secondary Payer determinations, Medicare’s “incident to” billing rules, and Medicare’s specific documentation requirements for different service categories. When processing a Medicare claim, staff access the Medicare library and use the appropriate Snippets.
Commercial payer libraries would include that payer’s prior authorization requirements, claim submission formatting requirements, appeal procedures and timelines, and contact information for common issues. When a claim involves a particular commercial payer, staff use that payer’s library.
This organization by payer dramatically reduces errors from confusion about requirements. Staff don’t need to remember whether Medicare or Blue Cross requires pre-authorization for MRI because they access the relevant payer library, and the Snippet tells them what’s required.
Week four should include practice scenarios that require using multiple payer-specific libraries, understanding how to quickly identify which payer’s requirements apply to a particular claim, and recognizing when payer requirements conflict with standard practices and require escalation to supervisors.
Ongoing training and continuous improvement
Training doesn’t end after the initial four weeks. The most successful billing teams commit to continuous learning and systematic improvement of their documentation practices.
Monthly continuing education sessions
Schedule regular continuing education sessions focused on recent payer policy changes that affect billing practices, new regulations or compliance requirements, analysis of recent denial patterns and prevention strategies, advanced TextExpander features and workflow optimizations, case studies of complex billing scenarios and how they were resolved, and updates to organizational policies or procedures.
These sessions keep staff current with the constantly changing billing landscape. They also provide opportunities for team members to share insights and learn from each other’s experiences. When one specialist discovers an effective approach to a common challenge, monthly training sessions allow that knowledge to spread to the entire team.
Think about bringing in external experts periodically. Representatives from major payers can explain recent policy changes and answer questions. Professional coders can provide advanced training on complex scenarios. Compliance specialists can review recent enforcement actions and discuss lessons learned.
Documentation of these training sessions serves dual purposes. It provides reference materials staff can revisit when needed, and it shows auditors and compliance reviewers that the organization invests in ongoing staff education, which is a positive signal of compliance commitment.
Tracking key performance indicators
Systematic tracking of billing performance metrics identifies improvement opportunities and measures training effectiveness. Essential KPIs for medical billing teams include clean claim rate or percentage of claims accepted on first submission, denial rate by reason code, average days in accounts receivable, collection rate as percentage of charges, and appeal success rate for denied claims.
Track these metrics both at the team level and for individual staff members. Team-level metrics reveal organizational trends and identify systemic issues. Individual metrics highlight training needs and recognize top performers.
When KPIs indicate problems, use the data to drive targeted interventions. If denial rates for a particular service type spike, conduct focused training on that service’s requirements. If one payer consistently denies claims at higher rates than others, review that payer’s specific requirements and update relevant Snippets.
Share KPI trends with the team regularly. Transparency about performance builds accountability and lets staff see the impact of their work. When the clean claim rate improves following implementation of new quality check Snippets, celebrating that success reinforces the value of systematic processes.
Adapting to industry changes
Healthcare billing regulations, payer policies, and technology standards change constantly. Organizations have to build adaptability into their training and documentation systems.
When Medicare announces policy changes, designate responsibility for reviewing the changes and determining impacts on your organization’s billing practices. This review should identify Snippets that need updating, new Snippets that should be created, and training topics that should be addressed in the next continuing education session.
Create a change management process for Snippet libraries. When significant updates are needed, communicate the changes to all staff before they take effect. Provide brief training on what’s changing and why. Update documentation that references the modified Snippets.
This systematic approach to change management ensures that organizational knowledge stays current. Instead of having some staff work from outdated information while others use current requirements, Snippet library updates make changes universally available immediately.
Think about creating a “recent changes” Snippet that staff can expand to see a summary of recent updates to Snippet libraries, recent payer policy changes affecting their work, and upcoming changes that will take effect soon. This single source keeps everyone informed without requiring attendance at meetings or review of lengthy policy documents.
Benefits of using TextExpander in medical billing training
Accelerated onboarding timeline
With TextExpander-enhanced training, organizations can significantly reduce onboarding timelines while achieving equal or better competency levels compared to traditional approaches.
This acceleration results from several factors. Snippet libraries provide instant access to organizational knowledge that would otherwise require months of exposure to learn. New staff can immediately use the same documentation approaches and language as experienced team members. They don’t need to memorize hundreds of codes, payer requirements, and processes because they know how to access the Snippet libraries that contain this information.
The reduced training time delivers substantial cost savings. Every week that a new hire operates at less than full productivity represents lost revenue and higher supervision costs. Significantly cutting training time means new staff contribute to organizational revenue sooner and require less intensive supervision.
Additionally, shorter training timelines make it easier to scale billing teams when needed. Organizations can respond to growth or staffing changes more quickly when they can bring new team members up to speed rapidly.
Consistent compliance and quality
Human memory fails. Even experienced billing specialists occasionally forget requirements or make transcription errors. TextExpander Snippets eliminate this source of error by ensuring that documentation consistently includes all required elements in the correct format.
This consistency becomes particularly valuable for maintaining compliance with complex regulations. When HIPAA requires specific elements in authorization releases, a Snippet ensures all elements are always present. When Medicare mandates particular documentation for Advance Beneficiary Notices, a Snippet generates compliant notices automatically.
Quality control becomes more effective when documentation follows predictable patterns. Supervisors reviewing claims can quickly spot deviations from standard approaches, which indicate errors. When documentation varies widely among staff members, identifying problems becomes much harder.
Organizations using Snippet-based documentation report measurably higher clean claim rates and lower denial rates. These improvements directly impact revenue because fewer denied claims mean faster payment and fewer resources spent on appeals and resubmissions.
Reduced claim denials and faster revenue collection
The financial impact of improved documentation accuracy extends throughout the revenue cycle. Claims submitted correctly the first time get paid faster. Organizations avoid the costs of reworking denied claims. Cash flow improves when payments arrive sooner.
Think about the math of a 5% improvement in clean claim rate for an organization processing 10,000 claims monthly. If 5% more claims are accepted on first submission, that’s 500 fewer denials to rework. At $25-50 per claim for rework costs, that represents $12,500 to $25,000 in monthly savings or $150,000 to $300,000 annually.
Beyond direct cost savings, faster payment improves organizational financial health. Healthcare providers operate on thin margins and depend on consistent cash flow. When claims get paid 30 days sooner because they’re submitted correctly initially, that acceleration in payment timing can meaningfully improve the organization’s financial position.
Institutional knowledge preservation
Healthcare organizations face constant staff turnover. When experienced billing specialists leave, they take valuable knowledge with them. Organizations then have to rebuild that expertise through expensive experience and training.
TextExpander Snippet libraries capture institutional knowledge in transferable format. When an expert billing specialist creates Snippets documenting her approach to complex payer requirements, that knowledge stays available to the organization even if she leaves. New staff can use those same Snippets, immediately operating at a higher level than they could without access to this expertise.
This knowledge preservation proves particularly valuable for rarely encountered but important scenarios. Most billing teams occasionally face unusual situations like rare diagnosis and procedure combinations, complex coordination of benefits scenarios, or appeals that escalate to unusual levels. When these situations arise once or twice per year, staff might not remember the details from previous occurrences. Well-documented Snippets preserve the knowledge of how to handle these situations.
Ready to reduce claim denials and accelerate training?
See how TextExpander helps healthcare organizations train billing teams faster while maintaining documentation accuracy that directly impacts revenue.
Integrating TextExpander with medical billing technology
Modern medical billing depends on integrated technology systems. TextExpander works alongside these systems to enhance rather than replace existing investments.
Seamless integration with practice management systems
TextExpander functions as a system-wide tool that works within any app where staff enter text. This universal compatibility means it integrates naturally with practice management systems, electronic health records, clearinghouse portals, payer authorization systems, and communication tools.
Staff use TextExpander to accelerate data entry in their practice management system. Instead of typing complete diagnosis codes, they use Snippet abbreviations that expand to full codes. Instead of manually entering patient demographic information, they use Snippets that insert standardized formats.
The integration doesn’t require technical configuration or API connections. Because TextExpander operates at the operating system level, it works in any app the staff member uses. This simplicity means organizations can implement TextExpander without involving IT departments in complex integration projects.
Enhancing EHR documentation workflows
Electronic health record systems contain the clinical documentation that supports medical billing. TextExpander helps billing staff work more effectively with EHR data by creating Snippets that extract relevant information from EHRs and format it for billing purposes, generating queries to providers when documentation is insufficient to support billing, and creating standardized notes in EHR systems that document billing-related communications.
While medical dictation software helps providers create clinical notes more efficiently, TextExpander focuses on standardizing and automating the billing and administrative documentation that flows from those clinical encounters. For organizations looking for clinical documentation templates like SOAP notes or patient visit summaries, TextExpander’s template library provides healthcare-specific starting points that can be customized for billing workflows.
For example, when a billing specialist reviews a provider’s note and identifies documentation gaps that prevent claim submission, they can use a TextExpander Snippet to generate a standardized query to the provider. The Snippet includes the patient name, date of service, specific documentation gap, and clear explanation of what additional documentation is needed. This standardization ensures queries are clear, professional, and consistently formatted.
Creating unified documentation standards across systems
Healthcare organizations use multiple systems that don’t communicate effectively with each other. A practice management system, EHR, billing system, and authorization tracking system might all require similar information entered in slightly different formats.
TextExpander Snippets can bridge these systems by providing consistent documentation that adapts to each system’s requirements. A Snippet might expand patient demographic information formatted for the practice management system, while a different Snippet expands the same information formatted for submission to a payer portal.
This approach reduces the redundant data entry that frustrates billing staff and introduces errors. Staff enter information once, then use Snippets to insert it in appropriate formats across different systems.
Expected outcomes from implementation
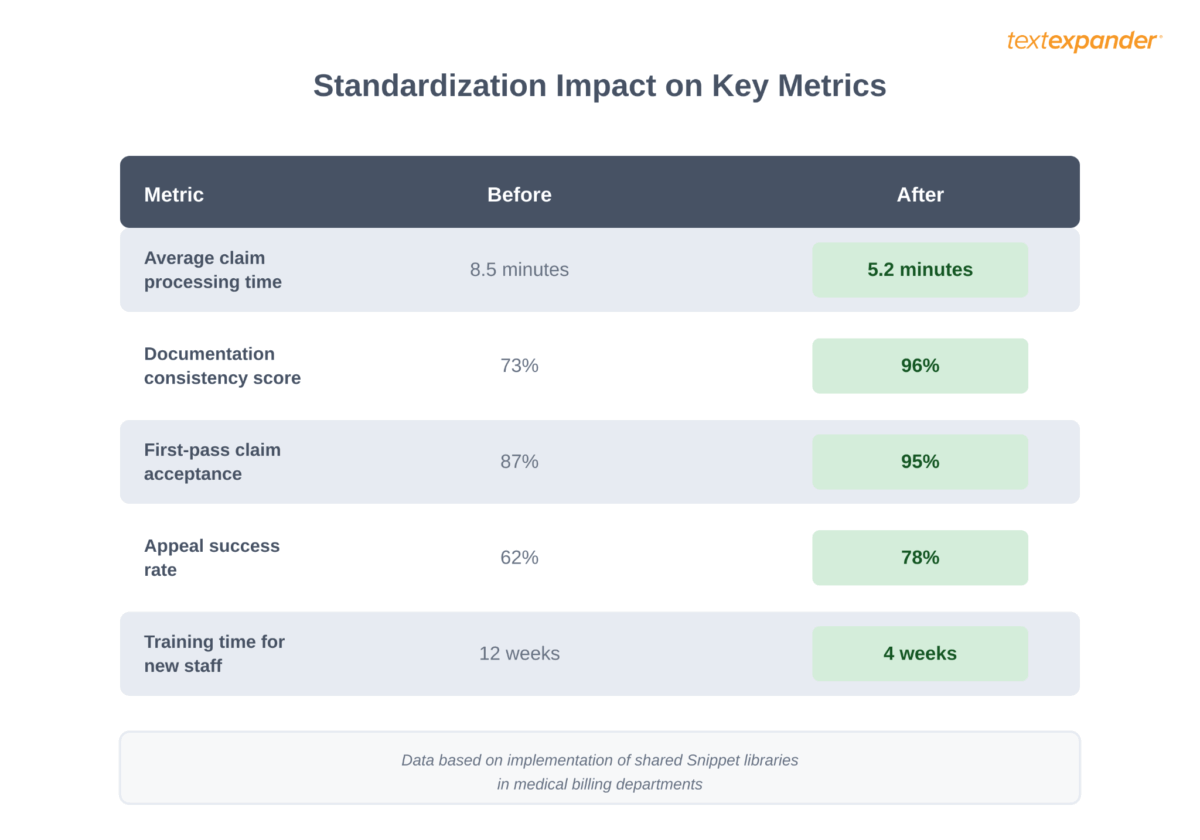
When healthcare organizations implement TextExpander-based training programs, they can expect measurable improvements across multiple dimensions. While specific results vary by organization size, baseline performance, and implementation approach, the following scenarios illustrate the types of outcomes organizations typically pursue.
Small practice scenario: Building consistency
Consider a small primary care practice with 3-5 providers and a billing team of 2-3 specialists. If each billing specialist has developed their own documentation approaches, inconsistency becomes inevitable. Different staff members handle the same scenarios differently, leading to varying outcomes and quality issues.
In this scenario, the practice might currently maintain a clean claim rate around 80-85%, which is below the industry benchmark of 95%. With 2,500-3,000 claims processed monthly, even a modest 8-10% improvement in clean claim rate would represent 200-300 fewer denials to rework each month.
Given rework costs of $25-50 per denied claim, this improvement could generate $5,000-15,000 in monthly operational savings. Beyond direct cost reduction, the practice would expect faster cash flow, reduced staff stress from handling fewer denial appeals, and improved ability to scale when adding new billing staff.
The implementation approach for a practice this size focuses on identifying the 15-20 most common billing scenarios and creating comprehensive Snippets for each, developing payer-specific libraries for their top insurance companies, and establishing shared documentation standards that eliminate variation among team members.
Multi-location organization scenario: Scaling best practices
Healthcare organizations operating multiple locations face particular challenges with consistency. When each location develops its own billing practices, performance varies widely. Some locations might maintain denial rates of 7-9%, while others struggle with 15-20% or higher.
For an organization with 8-12 clinic locations and 12-20 billing staff members, the opportunity lies in capturing what makes top performers successful and distributing that knowledge organization-wide. Rather than having expertise siloed at individual locations, Snippet libraries make best practices accessible everywhere.
The expected outcome centers on bringing all locations closer to the performance level of the best-performing sites. If organization-wide denial rates currently average 13-16%, reducing this to 8-10% through standardization could have substantial financial impact. For a system processing 15,000-20,000 claims monthly, each percentage point improvement in denial rate represents significant savings in rework costs and accelerated cash flow.
Implementation requires identifying top performers, documenting their approaches as Snippets, rolling out shared libraries across all locations, and establishing quality control processes that maintain consistency while allowing appropriate flexibility for site-specific needs.
Specialty practice scenario: Preserving critical expertise
Specialty practices face unique billing complexity. Oncology, cardiology, and other specialties deal with expensive medications requiring prior authorization, complex coding for varied treatment regimens, and extensive payer-specific requirements. This complexity means that billing expertise becomes concentrated in one or two senior specialists who understand the intricacies.
When a senior billing specialist leaves, the practice faces a knowledge crisis. Without that individual’s expertise, denial rates might spike, prior authorizations get delayed, and revenue suffers. Training a replacement traditionally requires 6-12 months of intensive mentoring to develop equivalent knowledge.
The opportunity lies in capturing expert knowledge in Snippet libraries before turnover occurs. When an experienced specialist’s approaches, payer-specific knowledge, and problem-solving techniques exist as documented Snippets, new hires gain immediate access to this expertise. Rather than starting from zero, they work from the foundation of institutional knowledge.
Expected outcomes include dramatically reduced risk from staff turnover, faster onboarding for replacement hires, maintained billing performance during transitions, and distributed expertise that prevents single points of failure in the billing operation.
See how affordable better training can be
TextExpander costs just a few hundred dollars annually for a billing team. Compare that to the cost of a single denied claim that requires rework.
Measuring Training Effectiveness and Business Impact
Training programs require measurement to justify investment and identify improvement opportunities. You need to track both leading indicators that predict success and lagging indicators that confirm outcomes. Without measurement, you can’t tell effective training from wasted time.
Establishing Pre-Training Baseline Metrics
Meaningful measurement requires understanding performance before training interventions. Collect baseline data for at least 90 days before implementing new training programs so you can demonstrate whether changes actually improve results or simply coincide with natural variation.
Clean claim rate measures the percentage of claims paid on first submission without requiring corrections or additional information. Organizations with weak training often see clean claim rates between 75-85%, while well-trained teams consistently achieve 90-95% clean claim rates per Healthcare Financial Management Association benchmarks. Calculate clean claim rate by dividing claims paid on first submission by total claims submitted during the period.
Denial rates by category reveal specific problem areas. Track denials separately for eligibility issues, coding errors, medical necessity questions, timely filing violations, and authorization problems. Overall denial rates increased from around 10% to nearly 12% industry-wide between 2020-2024, with many organizations experiencing even higher rates. Knowing which categories drive your denials focuses training on actual problem areas rather than generic improvement efforts.
Days in accounts receivable measures how quickly organizations collect payment. HFMA recommends maintaining days in A/R between 30-40 days, while MGMA suggests 40-50 days as acceptable performance. Calculate by dividing total accounts receivable by average daily charges. Higher days in A/R typically indicate claim submission delays, frequent denials requiring rework, or weak collections processes—all addressable through training.
Net collection rate shows what percentage of expected revenue the organization actually collects. Target rates above 95%, with best-performing organizations achieving 97-99%. Calculate by dividing actual collections by expected collections after contractual adjustments. Low collection rates often reflect training gaps in denial management, payment posting accuracy, or patient collections.
Cost per claim provides efficiency context. MGMA benchmarks suggest medical practices should target $3-7 per claim in processing costs depending on specialty and volume. Organizations with poorly trained staff incur higher costs through rework, extended processing times, and management oversight requirements. Tracking cost per claim demonstrates training’s financial impact beyond just revenue metrics.
Setting Realistic Improvement Targets
Training produces incremental improvement over time rather than overnight transformation. Set quarterly targets that reflect achievable progress while maintaining motivation through regular success.
Clean claim rate improvements typically progress from baseline through stepped improvements. An organization starting at 82% might target 85% after the first quarter of enhanced training, 88% after six months, and 92% by year-end. Each 3-5 percentage point improvement requires sustained effort and represents meaningful revenue cycle enhancement.
Denial rate reductions follow similar patterns. A team with 15% baseline denials might target 12% after initial training phases, 10% at six months, and 8% as a mature-program target. Every percentage point reduction represents thousands of dollars in saved rework costs and protected revenue.
Days in A/R improvements should target 5-7 day quarterly reductions. An organization at 62 days might aim for 55 days after quarter one, 48 days after quarter two, and 40-45 days as a sustained target. Rapid improvements suggest process problems beyond training, while gradual progress indicates building fundamental skill and knowledge.
Tracking Individual Staff Development
Organizational metrics reveal overall impact, but individual tracking shows how specific team members progress and identifies who needs additional support versus who’s ready for advanced responsibilities.
Track claim accuracy from day one showing the percentage of claims processed correctly without errors requiring correction. New staff typically achieve 60-70% accuracy initially, progressing to 85% by week 4, 90% by week 8, and 95%+ by weeks 10-12 as they gain proficiency. Staff not reaching these milestones by expected timeframes need intervention before problems solidify into habits.
Monitor task completion times to assess efficiency development. New staff require more time per claim, per payment posting, and per verification than experienced team members. Track how long standard tasks take and compare to team averages. Staff should approach average productivity by week 10-12, though peak efficiency often takes 6+ months.
Document error patterns to distinguish systematic knowledge gaps from careless mistakes. A staff member repeatedly making the same coding error needs targeted education on that specific topic, while someone making diverse unrelated errors needs to slow down and increase attention to detail. Different error patterns require different interventions.
Assess self-assessment accuracy by comparing what staff think they know to actual demonstration. Trainees who confidently claim competence despite making frequent errors need recalibration of their self-evaluation skills, while those who accurately identify their knowledge gaps show the self-awareness supporting continued development.
Monitoring Leading Indicators for Early Problem Detection
Lagging indicators like denial rates show what already happened, while leading indicators predict future problems before they fully manifest. Monitor these forward-looking metrics to intervene proactively rather than reactively.
Pre-submission scrubbing results from clearinghouses reveal potential claim problems before submission. Track the error rate on scrubbed claims and common error types identified before claims reach payers. Rising error rates during scrubbing suggest degrading claim quality even if denials haven’t increased yet due to correction before submission.
Prior authorization obtainment rates show whether staff secure approvals before service delivery. Track authorization requests submitted, approvals obtained, denials received, and services delivered without authorization when required. Declining authorization success rates predict future denials once claims submit.
Documentation query response time measures how quickly providers respond to requests for clarification or additional information. Faster responses speed up claim submission and reduce aging. Track days from query to response, percentage requiring multiple requests, and queries never answered. Persistent long response times indicate communication process problems worth addressing.
First-call resolution rate for patient financial inquiries demonstrates staff knowledge and problem-solving capability. Track what percentage of patient questions get resolved during initial contact versus requiring escalation, research, or callback. Low resolution rates suggest training gaps in customer service, systems knowledge, or problem-solving approaches.
Creating Performance Visualization and Reporting
Data means little if people can’t quickly understand what it shows. Create visual dashboards that make performance trends immediately apparent and accessible to both individual staff and team leaders.
Weekly performance summaries show each staff member their clean claim rate for the week, number of errors by category, completion time metrics compared to team average, and improvement trend from previous weeks. Simple bar charts or line graphs make trends obvious. Staff can immediately see whether their performance is improving, declining, or plateauing.
Monthly team scorecards display organizational metrics including clean claim rate trend line, denial rate by category with month-over-month changes, days in accounts receivable, net collection rate, and cost per claim processed. Scorecards create transparency about team performance and help everyone understand how individual work contributes to organizational outcomes.
Quarterly trend analysis compares current period to baseline and previous quarters across all major metrics. Identify areas of sustained improvement worth celebrating, metrics plateauing that need renewed focus, and any deteriorating performance requiring immediate intervention. Quarterly reviews provide appropriate perspective since billing metrics naturally fluctuate weekly but trends become clear over longer timeframes.
Reporting snippets that insert standard performance metrics into emails, meeting notes, and dashboards save time here. Templates ensure consistent reporting format while eliminating the tedious work of preparing routine performance summaries.
Connecting Training Investment to Business Outcomes
Training consumes time and resources, so demonstrating return on investment justifies continued support for development programs. Translate performance improvements into financial impact that resonates with organizational leadership.
When clean claim rate improvements reduce rework, calculate the cost savings. If enhanced training increased clean claim rate from 82% to 93%, that’s 11% fewer claims requiring correction. Multiply the reduction by total annual claim volume and average cost per claim correction to show dollar impact. A practice submitting 50,000 claims annually saves roughly $55,000 per year if corrections cost $10 each and 11% fewer claims need rework.
Calculate revenue protection from denial rate reductions. Every percentage point decrease in denial rates means less revenue at risk. If denial rates dropped from 14% to 9%, that’s 5% more claims paid on first submission. Multiply the improvement by gross charges to show revenue protected from denial risk. An organization billing $10 million annually protects $500,000 in revenue from denial risk with a 5% denial rate improvement.
Show retention value when trained staff stay longer than inadequately trained employees. Employee turnover costs include recruiting, hiring, training time, and productivity loss during ramp-up. Research from Premier Inc. shows that administrative costs per denied claim increased from $43.84 in 2022 to $57.23 in 2023, reflecting labor-intensive rework requirements. Industry data suggests replacing a medical biller costs $5,000-15,000 depending on role complexity. If enhanced training reduces turnover from 30% to 15% annually in a 10-person department, you prevent 1-2 terminations annually worth $10,000-30,000 in avoided costs.
Demonstrate faster time to productivity when structured training reduces weeks until independence. If new staff reach full productivity in 8 weeks instead of 14 weeks, the organization gains six weeks of productive work per hire. Multiply that across several hires annually to show meaningful capacity gains. Four new hires reaching productivity six weeks faster provides 24 weeks of additional billing capacity annually—equivalent to nearly half a full-time employee.
Calculate opportunity cost of management time saved when staff require less supervision. Experienced billers spending 10 hours weekly supervising undertrained staff can redirect that time to higher-value activities like denial prevention, process improvement, or strategic payer negotiations. Ten hours weekly across 50 weeks equals 500 hours annually, representing significant management capacity.ence tools embedded in their workflow.
Supervisor time required decreases as training becomes more systematic. When new staff can reference Snippet libraries rather than constantly asking questions, supervisors can focus on complex exceptions rather than basic guidance.
Quality and accuracy metrics
Clean claim rate or first-pass acceptance rate should improve steadily. Set organizational targets of 95% or higher and track progress toward that goal.
Denial rates by denial reason reveal specific training needs. If denials for missing prior authorization spike, additional training on authorization requirements is needed. If denials for incorrect coding increase, review coding training and relevant Snippets.
Appeal success rates indicate whether staff understand how to build effective appeals. High success rates show good training in payer policies and documentation requirements.
Financial impact metrics
Cost per claim including all labor and rework should decrease as efficiency improves and denial rates drop. Track this metric to quantify the ROI of training investments.
Days in accounts receivable should shorten as clean claim rates improve. Claims paid on first submission generate revenue 30-45 days faster than claims that require rework.
Net collection rate as percentage of charges should improve as fewer claims are written off due to untimely filing or inability to overcome denials.
Staff satisfaction and retention
Employee satisfaction scores among billing staff provide important feedback about training effectiveness. Staff who feel well-trained and supported by good tools report higher job satisfaction.
Turnover rate in the billing department should decrease. When staff feel confident in their abilities and have tools that make their work easier, they’re less likely to leave for other opportunities.
Error-related stress levels decline when staff have systematic approaches to prevent mistakes. Billing specialists cite stress from fear of making expensive errors as a major job dissatisfaction factor.
Getting started with TextExpander for medical billing training
Medical billing in 2026 demands more than traditional organizational onboarding can deliver. Certified professionals arrive with coding expertise, but then spend 30-90 days learning your systems, your payers, your workflows through shadowing and trial-and-error. Organizations face increasing complexity, rising denial rates with 41% of providers experiencing 10% or higher denial rates, staff shortages, and relentless pressure on margins. Success requires systematic approaches to organizational knowledge transfer: capturing payer-specific requirements, internal workflows, and institutional expertise so new team members become productive faster while maintaining the documentation accuracy that directly affects your revenue.
The four-week training framework outlined in this guide shows that rapid, effective training is achievable when organizations use modern automation tools alongside proven training methods. TextExpander’s Snippet libraries turn institutional knowledge from something that exists only in the minds of experienced staff members into accessible resources that new team members can immediately use.
The benefits extend well beyond training efficiency. Organizations implementing these approaches see measurably better financial outcomes through reduced denial rates, faster revenue collection, and lower costs per claim processed. They build more resilient teams where knowledge doesn’t depend on individual staff members and where cross-training happens naturally through shared documentation systems. They create stronger compliance postures with systematic documentation approaches that provide clear audit trails.
Perhaps most importantly, they position themselves for sustainable success in a challenging environment. As billing requirements grow more complex and staff turnover continues to challenge healthcare organizations, the ability to rapidly train new team members while maintaining quality becomes a competitive advantage.
The investment required is modest. TextExpander costs a few hundred dollars annually for a billing team. The time investment in building initial Snippet libraries pays returns immediately through reduced training time and improved accuracy. For organizations processing thousands of claims monthly, the financial returns from reduced denials alone exceed the investment within weeks.
Healthcare organizations that commit to modernizing their billing training approaches will find themselves better positioned to handle future challenges. Those that continue relying on traditional training methods (extended shadowing periods, memorization of endless requirements, and hoping new staff eventually develop expertise) will continue struggling with long training times, inconsistent quality, and preventable revenue loss.
The path forward is clear. Build systematic training approaches that use automation tools to speed up learning while improving quality. Capture institutional knowledge in shareable formats that make expertise broadly available. Create documentation systems that adapt quickly to changing requirements. Measure results systematically and refine approaches based on data.
When rolling out TextExpander-based training to your billing team, clear communication is essential. Use our training announcement email templates to inform staff about the new training program and set clear expectations for the implementation timeline.
Transform your medical billing training today
Join healthcare organizations that are training billing teams faster, reducing claim denials, and preserving institutional knowledge with TextExpander.
Frequently Asked Questions About Medical Billing Training
How long does medical billing training take?
Effective medical billing training typically takes 4-12 weeks for basic proficiency, with ongoing learning for advanced payer requirements and compliance updates. Our structured 4-week framework accelerates time to productivity compared to traditional 30-90 day onboarding approaches. Certified billing professionals already understand coding fundamentals, so organization-specific training focuses on your systems, payer mix, and internal workflows rather than teaching codes from scratch.
The training timeline breaks down as follows: Week 1 establishes organization-specific documentation workflows and introduces TextExpander Snippet libraries. Week 2 builds advanced automation skills with fill-in Snippets and shared team libraries. Week 3 emphasizes team collaboration and cross-training through shared documentation. Week 4 focuses on compliance requirements and quality standards. After initial training, staff work under supervision for 30-60 days before handling complex cases independently.
What are the most important skills for medical billing specialists?
Critical skills for medical billing specialists include medical coding proficiency across ICD-10-CM, CPT, and HCPCS code sets, understanding of payer-specific requirements and authorization processes, attention to documentation detail that supports billed service levels, knowledge of compliance regulations including HIPAA and False Claims Act requirements, and effective communication with providers when documentation gaps exist.
Beyond technical coding knowledge, successful billing specialists need analytical skills to identify denial patterns, problem-solving abilities for complex coordination of benefits scenarios, adaptability to frequently changing payer policies and regulations, and systematic approaches to quality control before claim submission. Organizations using TextExpander report that new staff develop these skills faster when they have instant access to institutional knowledge through Snippet libraries rather than relying solely on memory.
How can TextExpander improve medical billing training?
TextExpander accelerates training by providing new staff with pre-built templates for common documentation scenarios, ensuring consistency across the team regardless of experience level, and reducing cognitive load during the learning process by making expert knowledge instantly available. Organizations report reducing training time from 12 weeks to 4 weeks through systematic use of Snippet libraries.
The improvement comes from several factors: New staff can immediately use the same documentation approaches as experienced team members rather than developing their own methods. Snippet libraries capture payer-specific requirements that would otherwise take months of exposure to learn. Fill-in Snippets guide staff through complex workflows step-by-step, preventing missed requirements. Shared libraries mean that when one team member discovers a more effective approach, everyone benefits immediately through updated Snippets.
What’s the difference between certification and organizational training?
Medical billing certification provides foundational knowledge: understanding of code sets, basic compliance requirements, medical terminology, and standard billing concepts. This education typically takes 4-12 months through programs like Certified Professional Biller (CPB) or Certified Billing and Coding Specialist (CBCS).
Organizational training focuses on how YOUR specific practice operates: your practice management system configuration, your top payers’ unique requirements, your internal documentation standards, your escalation procedures for complex cases, and where your EHR stores specific information needed for billing. Certification teaches you WHAT a prior authorization is; organizational training teaches you exactly HOW your organization handles prior auth requests for each major payer in the formats they require. This organization-specific knowledge is what TextExpander Snippet libraries capture and make transferable.
How do I measure medical billing training effectiveness?
Measure training effectiveness through quantifiable metrics: clean claim rate above 95% (claims accepted on first submission), denial rate below 10% with specific tracking by denial reason, time to independent productivity measured in weeks, error rates in practice exercises and real claims, and staff retention through the first year. Compare these metrics before and after implementing structured training approaches.
Additionally track: average days in accounts receivable (should decrease as clean claim rates improve), appeal success rates for denied claims, supervisor time required for oversight (should decrease as training improves), and staff confidence levels through regular check-ins. Organizations using TextExpander-enhanced training report measurably higher clean claim rates and lower denial rates within the first 90 days compared to traditional training approaches.
What compliance requirements must medical billing training cover?
Medical billing training must cover federal healthcare regulations including Medicare and Medicaid policies, commercial payer contract requirements, HIPAA privacy and security rules for handling protected health information, and professional ethical standards that prohibit fraudulent billing practices.
Specific compliance topics include: medical necessity requirements that ensure all services billed are appropriate and documented, correct coding principles that prevent upcoding and unbundling, documentation standards that support billed service levels, understanding of fraud and abuse laws including the False Claims Act, proper use of modifiers and their compliance implications, and audit preparedness through systematic documentation practices. TextExpander Snippet libraries can embed compliance checks directly into workflows, ensuring staff verify required elements before claim submission rather than relying on memory.
How do I handle payer-specific requirements in training?
Managing dozens of different insurance payers with unique requirements is one of medical billing’s toughest challenges. Rather than expecting staff to memorize each payer’s quirks, create payer-specific TextExpander Snippet libraries that encode requirements into usable workflows.
A Medicare-specific library includes Snippets for Advance Beneficiary Notice requirements, Medicare Secondary Payer determinations, “incident to” billing rules, and Medicare’s documentation requirements for different service categories. Commercial payer libraries include each payer’s prior authorization requirements, claim submission formatting requirements, appeal procedures and timelines, and contact information for common issues. When processing a claim, staff access the relevant payer library and the Snippets guide them through requirements. This organization by payer dramatically reduces errors from requirement confusion.
Can TextExpander work with my existing practice management system?
Yes. TextExpander functions as a system-wide tool that works within any application where staff enter text, including practice management systems, electronic health records, clearinghouse portals, payer authorization websites, and email applications. The integration requires no technical configuration or API connections because TextExpander operates at the operating system level.
Staff use TextExpander to accelerate data entry in their practice management system through Snippet abbreviations that expand to complete codes or standardized formats. The tool doesn’t replace your existing systems but enhances how staff interact with them. Organizations can implement TextExpander without involving IT departments in complex integration projects, making it ideal for practices that want to improve efficiency without major technology investments.
What should be in a medical billing Snippet library?
A comprehensive medical billing Snippet library should include frequently used diagnosis and procedure code combinations for your organization’s most common encounters, standard responses to common payer documentation requests formatted to each payer’s requirements, patient demographic verification checklists that ensure complete information before claim submission, compliance reminders for high-risk services that frequently trigger denials, and payer-specific prior authorization request templates.
Advanced libraries include fill-in Snippets that guide staff through complex workflows like coordination of benefits for patients with multiple insurance policies, denial appeal letters at various escalation levels with payer-specific language, quality control checklists for claims before submission, and documentation query templates when provider notes don’t support billed service levels. Start with 15-20 essential Snippets covering your most common scenarios, then expand based on team feedback about situations where standardization would be valuable.
How do I keep Snippet libraries current with changing regulations?
Healthcare billing regulations and payer policies change constantly. Create a systematic change management process: designate subject matter experts responsible for monitoring changes in specific areas like Medicare policies or major commercial payer requirements. When changes are announced, these experts review impacts on your organization’s billing practices, identify Snippets that need updating, create new Snippets if needed, and communicate changes to all staff before they take effect.
Schedule quarterly reviews of entire Snippet libraries to identify outdated content. When significant updates occur, provide brief training on what’s changing and why. Update documentation that references modified Snippets. Consider creating a “recent changes” Snippet that staff can expand to see summaries of recent Snippet library updates, payer policy changes, and upcoming requirements. This systematic approach ensures organizational knowledge stays current rather than having some staff work from outdated information.
Key sources and references
2025 Experian Health State of Claims Report – Data on denial rates, causes of denials, and industry trends
Revenue Cycle Management in U.S. Healthcare – Umbrex – Comprehensive RCM analysis including denial trends and cost data
The Cost of Denial Management in Hospital RCM – Advantum Health – Cost per denied claim statistics
MGMA: You Might Be Losing Thousands of Dollars Per Month in “Unclean” Claims – Clean claim rate benchmarks
Medical Billing Mistakes Costing Healthcare Providers Millions in 2025 – Pena4 – Annual losses from billing errors

