Here’s the uncomfortable truth about healthcare billing departments right now: they’re barely keeping their heads above water. Experian Health’s 2025 State of Claims report found that 43% of revenue cycle management teams are understaffed. And it gets worse—research from Umbrex shows 33% of healthcare finance leaders say workforce shortages are their biggest operational headache.
You know what happens next. Overworked teams start making mistakes. Denials pile up. The pressure becomes unbearable.
But here’s what makes this crisis particularly painful: time. New billing staff need months to become fully productive. Not days. Not weeks. Months. And during that entire ramp-up period? Claims aren’t getting processed fast enough, your experienced staff are drowning under the extra workload, and cash flow starts to suffer. Add in payer requirements that seem to get more byzantine every quarter, plus regulatory changes that come faster than anyone can keep up with, and you’ve got a knowledge gap that just keeps growing.
The old approach doesn’t cut it anymore—you know, handing someone a three-ring binder and wishing them luck. Stakes are too high. The work is too complex. There’s no room for error when your margins are already razor-thin.
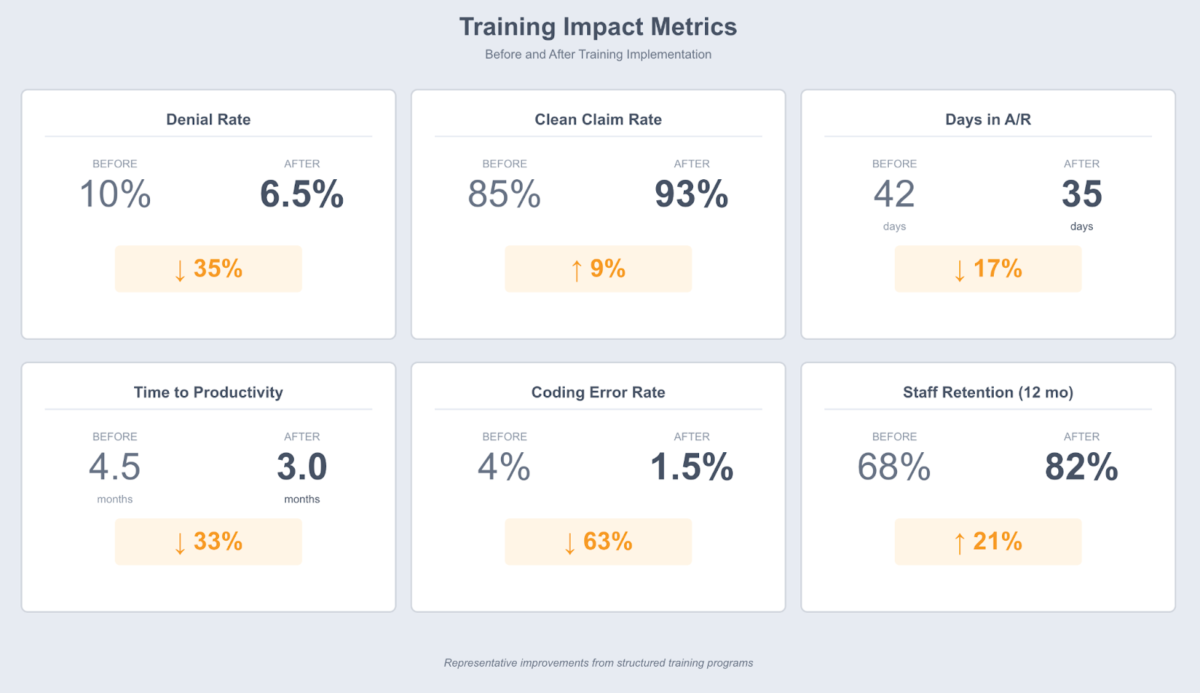
Organizations that actually invest in structured training programs? They’re seeing real results. Lower denial rates. New hires hitting productivity faster. Staff who stick around longer. Better financial performance across the board. Effective training is one crucial component of improving your overall medical billing process.
This guide gives you a practical framework for building training programs that work in the real world. We’re going to walk through everything from figuring out what your team actually needs to learn, all the way to setting up systems that keep knowledge current as the industry changes. Whether you’re training your very first billing employee or completely rebuilding how your department approaches professional development, you’ll find strategies you can use immediately—sized for your organization, applicable to your specialty, built for the challenges your team faces every day.
Free: Medical Billing Snippets
Download 27 TextExpander Snippets to help make your medical billing team more accurate and more consistent. Save time and reduce denied claims.
Understanding the Unique Challenges of Medical Billing Training
Let’s talk about why training billing staff is harder than training people in most other professional roles. It’s not just one thing—it’s everything at once. You’re dealing with regulatory compliance that carries real legal consequences. Technical coding knowledge that spans tens of thousands of codes. Insurance-specific requirements that vary wildly between payers. Financial processes that directly impact revenue. And all of this in an environment where the rules won’t stop changing and mistakes cost money immediately.
The staffing problem makes all of this worse. Way worse. Experian Health’s 2025 State of Claims report shows 60% of organizations have fewer than 25 people managing their entire claims process. When you’re already running lean and someone leaves or you’re trying to onboard someone new, it creates immediate pain. And when that experienced person walks out the door? They take years of institutional knowledge with them—all those mental shortcuts about specific payer quirks, workarounds for when systems don’t cooperate, hard-won understanding of what actually gets claims paid versus what the manual says should work.
New hires walk into a wall of complexity. They need to master the complete billing cycle from the moment a patient schedules an appointment through the final collection. Understand diagnosis and procedure coding systems with literally tens of thousands of codes. Learn the unique requirements of multiple insurance companies. Navigate compliance regulations where violations can destroy careers. Become proficient with specialized software that wasn’t exactly designed with user-friendliness in mind. There’s no shortcut through this knowledge base. The complexity guarantees mistakes during the learning period.
The payer requirement challenge deserves its own paragraph because billing staff consistently identify it as the most frustrating part of their job. Each insurance company has unique rules. Often each plan within a company has unique rules. One payer requires a specific modifier on a procedure code under certain circumstances. Another payer doesn’t. Medicare covers a preventive service annually. Commercial insurance covers it every two years. Authorization processes, appeal timelines, claim submission deadlines, documentation standards—all vary by payer. And keeping track of these differences isn’t just hard, it’s genuinely difficult even for experienced staff. Then payers update their policies with minimal notice, catching practices off guard and causing waves of denials that require urgent retraining.
Regulatory changes add another layer. When CMS issues new rules—changes to inpatient admission criteria, updates to documentation requirements, shifts in payment models—providers have to adapt fast or face denials and potential audits. Quarterly coding updates (CPT, ICD-10) need immediate incorporation into daily workflows. The pace of change means training can’t be a one-time event. It has to be ongoing, with mechanisms for rapid knowledge updates built in from the start.
The consequences of inadequate training show up fast in your operational metrics. Experian Health research indicates 90% of claim denials still require human review and rework before resubmission. According to the Medical Group Management Association (MGMA) and multiple industry analyses, each denied claim costs $25-50 to correct and resubmit. The cash flow delay adds indirect costs on top of that. When billing staff lack proper training, denial rates climb, days in accounts receivable stretch longer, and the organization’s financial health suffers. For healthcare providers operating on notoriously thin margins, these impacts can mean the difference between sustainable operations and financial distress. Organizations that invest in structured revenue cycle management training see measurably better outcomes across all these metrics.
Cross-training creates yet another dimension of complexity. When key billing functions depend on single individuals, vacation schedules and sick leave create immediate coverage gaps. Unexpected turnover? Even worse. Organizations with cross-trained staff handle these situations better, but building that depth of knowledge requires significant training investment. The alternative—being unable to submit claims because your authorization specialist called in sick—isn’t really viable.
Assessing Training Needs for Medical Billing Staff
Good training programs start by figuring out what your team actually needs to learn. Sounds obvious, right? But a proper skills assessment prevents you from wasting time teaching people things they already know while accidentally missing critical gaps. The assessment process looks different depending on whether you’re training completely new hires, bringing in experienced billers from other organizations, or upskilling your existing team on new requirements.
For brand new hires, you’re starting from zero. You need to assess their baseline knowledge across all the core competencies: Do they understand the healthcare billing cycle? Any familiarity with medical terminology? Prior coding experience? Have they worked with EHR or practice management systems before? What do they know about compliance requirements? How much do they understand about insurance processes? And here’s a trap—don’t assume prior healthcare experience translates to billing knowledge. A former medical assistant might have excellent clinical knowledge but know absolutely nothing about claim submission workflows.
When you’re onboarding experienced billers from other organizations, the challenge shifts. You’re trying to identify what’s different from their previous experience. They might be highly competent with certain payers but have never touched your organization’s specific contracts. Expert with one EHR system but need training on yours. Comfortable with certain specialties but require education on your service lines. A skills assessment matrix helps you map what they know against what your environment actually requires.
For existing staff, performance data becomes your most valuable assessment tool. Review recent denial reasons to identify systematic knowledge gaps. Authorization denials climbing? That signals a training need around pre-certification processes. Medical necessity denials increasing? Documentation education might be required. Coding error patterns reveal specific areas where staff need refresher training or deeper instruction.
Create a structured approach to skills assessment covering these key domains: Complete billing cycle knowledge (can they explain each step from pre-registration through payment posting?). Coding proficiency across relevant code sets (ICD-10-CM for diagnoses, CPT for procedures, HCPCS for supplies and services). Payer-specific requirements for your major contracts (Medicare/Medicaid rules, commercial payer policies, specialty plan requirements). Compliance awareness (HIPAA, False Claims Act, Anti-Kickback Statute, Stark Law). Software competency with your specific systems.
The payer knowledge assessment deserves special attention. Create a matrix mapping which staff members understand which payer requirements. If only one person can work Blue Cross claims because they’re the only one who understands that payer’s modifier requirements, you’ve just identified both a knowledge gap and an operational risk. The goal isn’t for everyone to be expert on every payer—that’s unrealistic. But you need enough depth that departures don’t cripple operations.
Don’t overlook assessing how well staff handle regulatory changes. Do they proactively monitor coding updates and payer policy bulletins? Or do they reactively discover changes through claim denials? Staff who don’t know where to find authoritative update sources (CMS, AMA, payer newsletters) or how to interpret them need training on staying current, not just training on current requirements.
Use a combination of assessment methods for the most accurate picture: written knowledge tests for compliance and coding fundamentals, practical claim coding exercises using actual scenarios, scenario-based questions about payer requirements and problem-solving, system proficiency tests for software competencies, and structured interviews to assess judgment and critical thinking. The investment in thorough assessment pays off by ensuring your training curriculum targets actual needs rather than assumed gaps.
Document your findings in a format that guides curriculum development. A simple table works well:
Knowledge Area | Current Competency | Target Competency | Training Priority | Timeline
For example: “Medicare billing rules | Basic understanding | Can submit clean Medicare claims independently | High | Weeks 2-4”
This assessment becomes your training roadmap. It ensures you address the most critical gaps first while providing a clear progression path for building comprehensive billing competency.
Aligning Training Objectives with Organizational Goals
Training programs need measurable objectives that connect directly to business outcomes. Without this alignment, training becomes an activity you do rather than an investment that drives results. The most effective training programs establish clear KPIs that leadership cares about and can see improving as staff complete training.
Start by articulating how specific training objectives support operational and financial goals. If your organization struggles with high denial rates, frame training objectives around denial reduction: “Reduce coding errors by 25% within 90 days” connects to “Decrease denial rate from 8% to 6%,” which translates to concrete revenue impact. If cash flow is your primary concern, training objectives might focus on accelerating claim submission: “Improve first-pass acceptance rate from 85% to 92%” directly impacts days in accounts receivable.
Establish baseline metrics before training begins so you can measure improvement objectively. Track key performance indicators including claim denial rate (overall and by denial reason), clean claim rate (percentage accepted on first submission), average days in accounts receivable, net collection rate (percentage of collectible revenue actually collected), coding error rate, and time-to-independence for new hires. These metrics provide clear evidence of training effectiveness and help justify continued investment in professional development.
Create a table that maps training objectives to business outcomes and success metrics. This framework helps you design curriculum that directly addresses organizational priorities:
- Training Objective: Master Medicare billing rules
- Business Goal: Reduce Medicare denials
- Success Metric: Medicare denial rate
- Target: <5% within 6 months
- Training Objective: Understand proper modifier usage
- Business Goal: Improve coding accuracy
- Success Metric: Coding error rate
- Target: <2% within 90 days
- Training Objective: Learn payer-specific authorization requirements
- Business Goal: Accelerate claims processing
- Success Metric: First-pass acceptance rate
- Target: >90% within 4 months
This explicit connection between training and business results helps secure leadership buy-in and resource allocation. When you can demonstrate that training investment improves financial performance, it becomes much easier to protect training time and budget against competing operational demands.
Present training as an investment with clear ROI. The math is straightforward: if your organization denies 100 claims monthly at an average rework cost of $35 per claim, that’s $3,500 in monthly denial management costs. Training that reduces denials by 30% saves $1,050 monthly—$12,600 annually. Compare that to the cost of developing and delivering the training program, and the business case becomes compelling.
Beyond financial metrics, consider retention impacts. Organizations that invest in professional development see improved employee retention, and the cost of turnover in billing positions is substantial. Industry research indicates that staff turnover in medical billing averages around 25% annually, with replacement costs ranging from $15,000-25,000 per position when factoring in recruitment costs, onboarding time, and the months of reduced productivity before new hires reach full competency. Training that improves job satisfaction and career development opportunities directly impacts retention economics.
Securing executive sponsorship requires demonstrating alignment between training outcomes and organizational strategy. If your CFO’s top priority is improving cash flow, emphasize how training accelerates claim submission and reduces denial-driven delays. If your compliance officer worries about audit risk, highlight how comprehensive compliance training reduces that exposure. Frame training in terms that resonate with each stakeholder’s priorities.
Establish accountability structures that ensure training follows through to operational improvement. Assign executive sponsors who receive regular updates on training metrics and outcomes. Include training-related goals in manager performance evaluations—completing staff training on schedule, achieving team competency standards, and improving relevant operational metrics. Create reporting cadences where training outcomes are reviewed by leadership alongside other financial and operational performance indicators.
The goal isn’t just to train staff but to demonstrably improve operational performance through training. When training objectives align tightly with business goals and you measure progress consistently, the value becomes undeniable and continued investment becomes an easy decision.
Accelerate Training with Instant Access to Billing Knowledge
Stop losing productivity while staff search for payer requirements and authorization processes. TextExpander gives your team instant access to billing templates, compliance checklists, and payer-specific workflows.
Developing Modular and Comprehensive Training Content
Break your training content into self-contained modules. Each one should let staff focus on mastering one competency at a time. Why modular? Because it works better for everyone. New hires can progress through foundational topics before tackling complex scenarios. Experienced staff can jump to specific modules for refreshers without sitting through stuff they already know. And when regulations or payer policies change (spoiler: they will), you’re updating discrete modules instead of overhauling your entire program.
Design your curriculum around core modules covering the complete knowledge base billing staff actually need. Here’s what a comprehensive program typically includes:
Foundations of medical billing covers the complete revenue cycle from pre-registration through payment posting, how clinical documentation connects to billing, basic insurance concepts and terminology, and an introduction to major payer types and their general requirements. This module ensures everyone shares a common understanding of how healthcare billing works before diving into specifics (trust me, they don’t).
Insurance verification and authorization training addresses how to verify eligibility and benefits effectively, understand coverage limitations and exclusions, navigate prior authorization requirements, recognize when referrals are needed, and document everything properly. Many claim denials trace straight back to inadequate front-end processes—this module is critical.
Medical coding fundamentals must cover diagnosis coding with ICD-10-CM (coding conventions, combination codes, documentation requirements), procedure coding with CPT and HCPCS (surgical procedures, E/M services, ancillary services), proper code linkage demonstrating medical necessity, and appropriate modifier use. Code selection directly impacts whether claims get paid. Coding proficiency isn’t optional. Documentation quality directly impacts coding accuracy, making clinical documentation improvement a critical adjacent competency for billing teams.
Claim submission and scrubbing training teaches how to prepare clean claims with all required data elements, understand claim forms (CMS-1500, UB-04) and electronic formats, use claim scrubbing tools to catch errors before submission, and recognize what different claim rejection and denial reasons actually mean. Staff need to understand not just how to submit claims but how to ensure they’re clean before they go out.
Denial management and appeals covers analyzing denial reasons and identifying patterns, distinguishing between denials needing clinical information versus administrative corrections, writing effective appeals with appropriate supporting documentation, understanding payer-specific appeal processes and timelines, and tracking denial trends to implement prevention strategies. Denials are inevitable. How you handle them determines whether you recover that revenue.
Payment posting and reconciliation training includes posting payments accurately and identifying underpayments, reconciling remittance advice with claims submitted, understanding contractual adjustments versus write-offs, recognizing when to appeal payment amounts, and handling refund situations properly. Accurate payment posting ensures your A/R data reflects reality instead of wishful thinking.
Collections and patient responsibility addresses communicating with patients about their financial responsibility, setting up payment plans and handling hardship situations, knowing when and how to send accounts to collections, using patient-friendly communication approaches, and maintaining compliance with debt collection regulations. With higher patient responsibility becoming the norm, this competency matters more every year.
Compliance and regulatory requirements must cover HIPAA privacy and security rules in billing contexts, the False Claims Act and fraud prevention, Anti-Kickback Statute and Stark Law basics, proper handling of overpayments and refunds, and documentation standards for audit readiness. Compliance violations carry career-ending consequences. This training is absolutely essential.
Within the coding module, develop dedicated content for payer-specific requirements. Each major payer your organization works with should have its own sub-module: unique billing rules, common denial reasons, modifier requirements, authorization workflows, claim submission deadlines, and appeal processes. When payers update policies (and they love to do this with minimal notice), you update their specific module instead of hunting through general content trying to find all mentions of that payer.
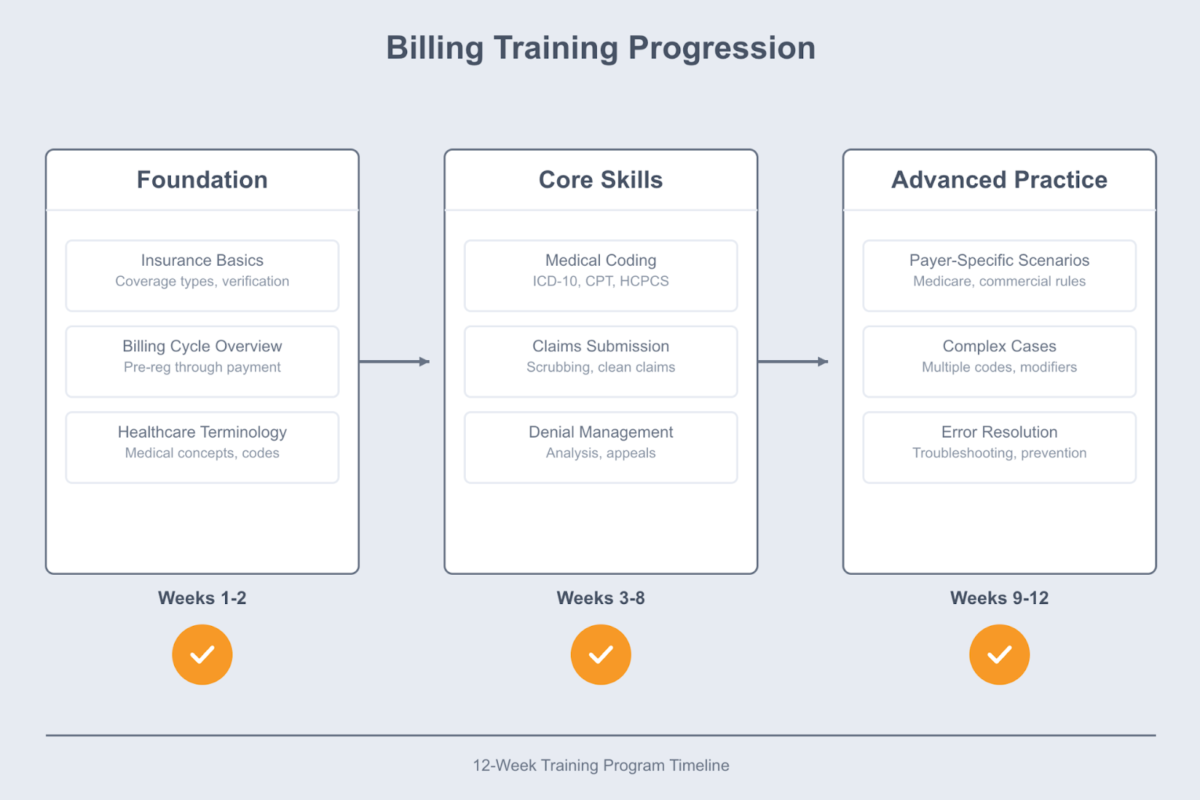
Create learning paths guiding staff through appropriate progressions. New hires might follow: Week 1-2 (Foundations and terminology) → Week 3-4 (Insurance verification and authorization) → Week 5-7 (Medical coding fundamentals) → Week 8-9 (Claim submission processes) → Week 10-11 (Denial management) → Week 12 (Payment posting and collections). Experienced staff transferring from other organizations might skip foundations and focus on your organization’s specific payers, systems, and specialties.
Design modules with clear learning objectives stated at the beginning, concrete content addressing those objectives, knowledge checks assessing comprehension, and practical exercises requiring them to apply what they learned. Each module should feel complete and self-contained while building toward comprehensive billing competency.
Build flexibility into your modular system. When regulatory changes occur, create brief update modules staff complete as urgent required training: “ICD-10 Quarterly Updates – Q4 2024” or “Medicare Two-Midnight Rule Changes – Effective 2025.” These focused modules keep your team current without requiring wholesale curriculum redesign.
Consider creating quick-reference materials accompanying each module: one-page workflow diagrams, checklists of required elements, tables of payer-specific requirements, job aids for common scenarios. Staff reference these materials during actual work, reinforcing training and reducing errors.
The modular approach also supports different learning paces. Some staff absorb coding concepts quickly and need more time on payer requirements; others struggle with coding but excel at patient communication. Modular design allows individualized progression while maintaining consistent standards for what everyone must know.
Integrating Real-World Scenarios and Hands-On Practice
Theoretical knowledge about billing rules means little if staff can’t apply it to actual claims. The gap between knowing what should happen and successfully navigating the messy reality of incomplete documentation, ambiguous payer policies, and system limitations is where most training fails. Effective training programs bridge this gap through extensive hands-on practice with realistic scenarios.
Start with actual claim examples from your organization, appropriately de-identified. Walk trainees through complete claim scenarios: review the clinical documentation, identify the appropriate diagnosis and procedure codes, verify insurance information, check for authorization requirements, prepare the claim, and anticipate potential denial reasons. Use claims that represent your actual case mix—if you’re a cardiology practice, trainees need practice with cardiac procedure coding; if you’re a skilled nursing facility, they need experience with therapy billing and Medicare Part A vs. Part B determinations.
Create graduated complexity in your practice scenarios. Begin with straightforward single-procedure visits with clear documentation and straightforward insurance coverage. Progress to more complex situations: multiple procedures requiring modifier usage, services with medical necessity concerns, cases involving coordination of benefits, claims requiring special handling per payer requirements, and scenarios with documentation deficiencies that need query processes. This progression builds confidence and competency systematically.
Develop error identification exercises using real denied claims. Present the original claim, the denial reason, and all available documentation, then have trainees identify what went wrong, determine the correct approach, gather any additional information needed, and practice submitting the corrected claim or writing an appeal. Use actual denial letters and EOB formats so trainees learn to interpret the language different payers use.
Set up practice environments where trainees can work with billing software without affecting production data. Most practice management systems support training databases where staff can submit test claims, post payments, work denials, and navigate workflows under supervision. This hands-on system experience is invaluable—reading about how to submit a claim is very different from actually doing it.
Include simulation of the complete patient encounter workflow. Have trainees role-play patient registration conversations, practice verifying insurance, determine if services need authorization, document the encounter appropriately, and code the claim. This end-to-end practice helps staff understand how errors at any stage impact downstream processes.
Create scenario-based exercises around the most common errors in your organization. If you frequently see incorrect place of service coding, design exercises that require identifying the appropriate place of service for different scenarios. If authorization lapses are a problem, practice scenarios where trainees must recognize when services need authorization and navigate the process. Target training to your actual pain points.
Address compliance and ethical decision-making through discussion-based scenarios. Present situations with ethical ambiguity: a physician pressures the coding team to select codes that maximize reimbursement but aren’t fully supported by documentation, a patient requests billing a covered service when they actually received a non-covered service, documentation is missing but the procedure was definitely performed. Use these scenarios to develop judgment about when to push back, when to seek clarification, and when to escalate concerns.
Incorporate payer-specific scenarios that highlight the differences between insurers. Present the same basic service but vary the payer, then have trainees identify what changes: different authorization requirements, different modifier needs, different documentation standards, different appeal processes. This comparative approach helps staff internalize that “it depends on the payer” isn’t an excuse but rather the reality they must navigate.
Use peer learning approaches where trainees work through scenarios in small groups, discuss their reasoning, and learn from each other’s perspectives. Multiple people examining the same claim scenario often identify different issues, and the discussion helps everyone develop more thorough analysis skills.
Provide immediate feedback on practice exercises. When trainees make errors, explain why their approach was incorrect, what the correct approach should be, what the consequences of the error would be in production, and how they can avoid that error in the future. Constructive feedback turns mistakes into learning opportunities.
Consider creating a library of 50-100 practice scenarios covering your most common billing situations. New hires work through these systematically during training. Experienced staff can use them for skills refreshment or when they’re learning to work a new payer or specialty. Build the library over time, adding new scenarios whenever you encounter unusual situations or new denial patterns.
The investment in realistic practice pays off dramatically. Staff who’ve worked through dozens of practice scenarios before touching production claims make fewer errors, solve problems more independently, and reach full productivity faster than those who receive only theoretical instruction.
Building Training Infrastructure for Scalable Success
Effective training programs need supporting infrastructure that makes knowledge accessible, consistent, and maintainable. Without proper systems and resources, training becomes dependent on individual trainers’ availability and knowledge, doesn’t scale as the organization grows, and degrades over time as content becomes outdated.
Develop comprehensive training documentation that staff can reference during and after formal training. Create detailed training manuals for each major topic area with step-by-step workflows, screenshots of system processes, explanations of requirements and rationale, and examples of correct and incorrect approaches. The manuals become the authoritative reference for how your organization handles billing processes.
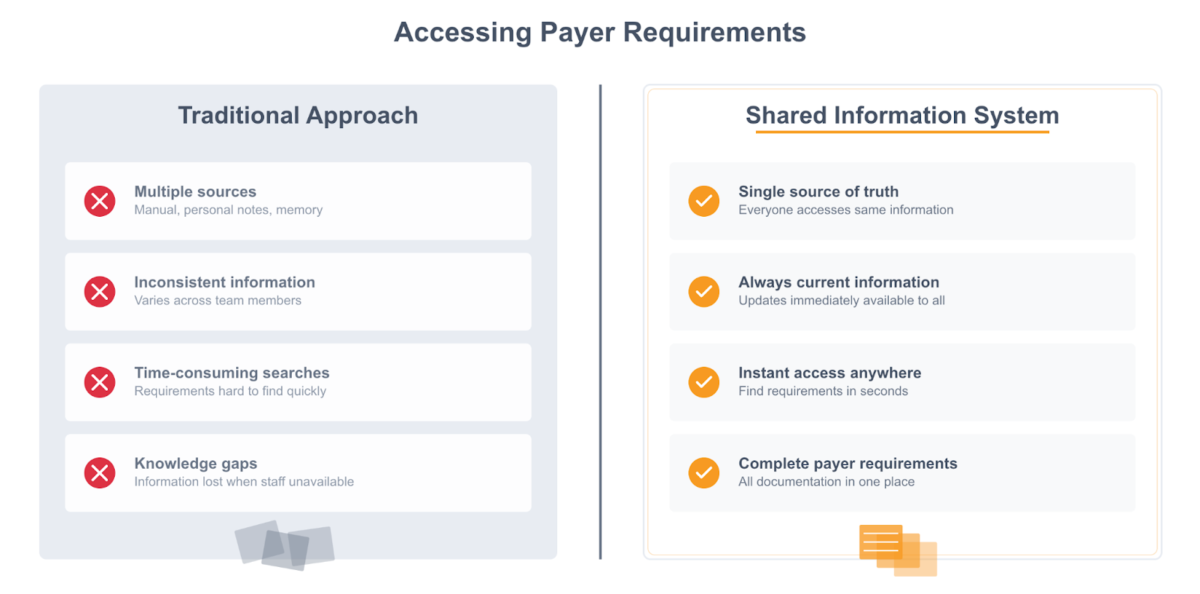
Organize documentation by function and payer so staff can quickly find what they need. If someone needs to submit a Blue Cross claim and can’t remember the modifier requirements, they should be able to find that information in under a minute. Structure your documentation library logically: by payer (Medicare, Medicaid, Blue Cross, United, Aetna), by function (verification, authorization, coding, submission, appeals), by specialty or service type (surgery, evaluation and management, ancillary services), and by situation (new patient visits, follow-ups, complex cases).
Implement a centralized knowledge base that’s searchable and accessible from anywhere staff work. Whether someone is in the office, working remotely, or covering an unfamiliar function, they need instant access to current procedures, payer requirements, regulatory guidelines, and troubleshooting help. Knowledge bases serve as institutional memory that persists regardless of staff turnover.
Include practical troubleshooting guides in your knowledge base: what to do when claims reject with specific error codes, how to handle situations when authorization can’t be obtained, steps to take when documentation is incomplete, processes for researching unfamiliar payer requirements, and escalation paths for situations requiring supervisor input. Staff facing challenging situations need quick answers, not lengthy manual searching.
Maintain strict version control and clearly mark when documentation was last updated. Nothing erodes trust in training resources faster than following documented procedures only to discover they’re outdated. Assign ownership for each documentation section to specific individuals responsible for monitoring changes and updating content. When a payer updates its policies, the person responsible for that payer’s documentation updates it immediately and notifies the team.
Create quick-reference materials for high-frequency tasks: laminated desk references with common codes, one-page workflows for routine processes, payer requirement summary sheets, and checklists for claim submission requirements. These job aids reinforce training and reduce errors during daily work. Many organizations find that shared snippet libraries serve this function particularly well—staff can access current templates, payer requirements, and authorization processes instantly without searching through documentation.
Implement cross-training programs that build depth across your team. Create a skills matrix showing which staff members are trained and proficient in each billing function and payer type. Identify gaps where only one person can handle critical functions, then systematically cross-train others to build redundancy. When your authorization specialist takes vacation or leaves unexpectedly, having others who can cover that function prevents operational disruption.
Design rotation schedules that allow staff to develop competency in functions adjacent to their primary role. A claims submission specialist might spend one week monthly working on denials, giving them insight into what causes denials and how their work impacts downstream processes. This rotation builds broader understanding while creating coverage capability.
Address the specific challenges of training remote and distributed teams. If you have offshore, nearshore, or remote billing staff, ensure they have equal access to training resources and support. Conduct training via video conferencing for live instruction, record sessions so remote staff can review them on-demand, use screen-sharing for software training and troubleshooting, establish virtual office hours for questions and coaching, and create detailed written procedures with screenshots that support self-guided learning. Organizations implementing productivity tools across distributed teams need clear onboarding processes for new staff to ensure consistent adoption regardless of location.
Consider time zone differences when scheduling live training for distributed teams. If simultaneous participation isn’t possible, record sessions and schedule follow-up Q&A sessions at times that work for different locations. Use asynchronous communication tools effectively—discussion forums where staff can ask questions and receive responses, shared documentation that everyone can access regardless of location, and collaboration platforms that support workflow coordination across time zones.
Build feedback and continuous improvement loops into your training infrastructure. Create mechanisms for trainees to provide input on training effectiveness, clarity, and gaps. Establish processes for trainers and supervisors to report common questions, confusion points, and areas where trainees consistently struggle. Schedule quarterly training program reviews where you assess what’s working and what needs adjustment. Use post-training performance data to identify topics requiring stronger emphasis or different teaching approaches.
The infrastructure investment pays off through consistency, scalability, and sustainability. When training resources are well-organized and accessible, new trainers can step in without complete reinvention. When staff can find answers independently, they interrupt supervisors less frequently. When knowledge is preserved in systems rather than residing only in people’s heads, staff turnover doesn’t devastate operations.
Choosing Effective Training Methods and Technologies
Different topics and learning objectives benefit from different instructional approaches. The most effective training programs combine multiple methods to accommodate various learning preferences, fit within operational constraints, and maximize both engagement and knowledge retention.
E-learning modules work particularly well for foundational knowledge that doesn’t require live instruction or immediate feedback. Compliance training, basic terminology, insurance concepts, and coding fundamentals can be delivered effectively through self-paced online courses. Staff complete them on their own schedule without taking trainers away from other responsibilities. Interactive elements within e-learning—knowledge checks, drag-and-drop exercises, scenario-based decision-making—keep learners engaged and reinforce key concepts.
Live instructor-led workshops excel for complex topics that benefit from discussion, immediate question-answering, and group learning. Topics like medical necessity determinations, complex coding scenarios, appeal writing, and ethical decision-making work well in workshop format where participants can ask questions, debate approaches, and learn from peer perspectives. The interaction and dynamic discussion add value beyond what self-paced modules provide.
One-on-one mentorship and shadowing provide personalized learning that adapts to individual needs. Pair new hires with experienced billing staff for structured mentorship during onboarding. Create shadowing opportunities where trainees observe mentors handling live work before attempting it themselves. Establish graduated responsibility where trainees begin with simpler claims and progress to complex cases as competency develops. Schedule regular check-ins where mentors review trainee work and provide constructive feedback.
Hands-on practice with actual billing software is non-negotiable for system competency. Staff need practice submitting claims, posting payments, working denials, and navigating your specific systems. Set up sandbox environments or test databases where trainees can practice without affecting production data. Create guided walkthroughs for common workflows with detailed steps and screenshots, then allow supervised practice where trainees complete tasks independently while trainers observe and assist.
Blended learning combines online knowledge acquisition with in-person application and discussion. Staff complete e-learning prerequisites covering factual content, then attend instructor-led sessions focused on applying that knowledge to realistic scenarios. This flipped classroom approach maximizes the value of expensive instructor time while ensuring staff come prepared to engage with complex material. The combination of independent learning and interactive practice tends to produce better outcomes than either approach alone.
Leverage technology appropriately for your training needs. Learning management systems organize course content, track completion, and administer assessments automatically. Video recording enables trainers to create content once and reuse it many times. Screen recording tools allow capture of system workflows and processes. Virtual meeting platforms enable remote training and support distributed teams. Collaboration tools facilitate ongoing learning and support after formal training concludes.
Don’t overlook low-tech training approaches that still work well. Lunch-and-learn sessions during team meals address topics in a casual, low-pressure environment. Brief daily huddles provide opportunities for quick knowledge sharing and question-answering. Rotating leadership of team meetings creates teaching opportunities where staff present topics to colleagues. Posting visual reminders and job aids around the workspace keeps critical information visible.
Create opportunities for staff to teach each other. When someone attends external training or masters a new skill, have them present what they learned to the team. Teaching others reinforces the presenter’s knowledge while spreading expertise throughout the department. This peer teaching approach builds team cohesion and creates a culture of continuous learning.
Consider gamification elements to increase motivation and engagement. Progress tracking shows staff how they’re advancing through training curriculum. Achievement recognition celebrates milestone completions. Friendly competition around assessment scores or error rates can motivate performance improvement. These game-like elements tap into natural human psychology around achievement and recognition.
Balance training time with operational needs. Protect dedicated training hours where staff aren’t pulled for operational work—otherwise, training constantly gets postponed for “urgent” needs. Consider staggered schedules where only part of the team trains at once, maintaining operational coverage. Use slack periods (if you have them) for intensive training blocks. Build training time into the work week rather than treating it as an extra burden on top of full workloads.
Evaluate which training methods work best for your organization based on outcomes, not just convenience. Track whether staff trained through e-learning perform as well as those who receive instructor-led training. Compare the speed to competency for different instructional approaches. Assess staff satisfaction and engagement with various training formats. Use this data to refine your training approach over time, investing more in what works and eliminating what doesn’t deliver results.
The right mix of training methods depends on your content, learners, resources, and constraints. Most organizations find that variety works better than relying on a single approach—different staff learn differently, different topics require different instruction, and different situations call for different solutions. Build a toolkit of training methods and choose appropriately for each situation.
See How Affordable Better Training Outcomes Can Be
TextExpander costs just a few hundred dollars annually per user. Compare that to the $25-50 cost of reworking each denied claim, or the months of reduced productivity while new hires learn payer requirements the hard way.
Leveraging Productivity Tools to Standardize Training Delivery
One of the biggest challenges in billing training is managing the sheer volume of detailed, constantly changing information that staff must access quickly. Payer requirements, authorization workflows, compliance reminders, documentation standards, and billing templates—staff need this information at their fingertips during actual work, not buried in manuals they have to search through.
Productivity tools that centralize and standardize access to critical information transform both training effectiveness and ongoing performance. The challenge isn’t just teaching staff the billing requirements—it’s ensuring they can recall or access those requirements accurately months later when they’re working an unfamiliar payer or handling a situation they haven’t encountered in weeks.
Consider the common scenario: a billing specialist needs to submit a claim to Blue Cross Blue Shield for a particular procedure. They learned in training that this payer requires specific modifiers under certain circumstances, has particular authorization requirements, and needs claims submitted within specific timeframes. But that training was three months ago, they’ve worked hundreds of other claims since then, and they can’t quite remember the exact requirements. They could search through documentation, ask a coworker, or make their best guess—but all of these approaches introduce delay, inconsistency, or error risk.
Shared snippet libraries solve this problem by giving staff instant access to current information. Instead of searching or relying on memory, they access the standardized Blue Cross requirements immediately: the required modifiers, the authorization process with specific phone numbers and turnaround times, the claim submission deadline, and the appeal process if the claim is denied. The information is identical for every team member because it comes from a centralized source, and when Blue Cross updates its policies, updating the central snippet ensures everyone immediately has current information.
This approach addresses one of billing’s most persistent pain points—the “mosaic of different payer requirements” that staff struggle to manage. Rather than each team member maintaining personal notes or relying on memory about individual payer quirks, shared snippets create a single source of truth. New hires access the same accurate information as experienced staff, reducing the knowledge gap and accelerating their productivity.
For payer-specific requirements, snippet-based access provides immediate value. A snippet for authorization requirements might include: the payer name and procedure types requiring authorization, the authorization request process with contact information, the documentation required for submission, the turnaround time for approval, and what to do if authorization is denied or delayed. Staff access this complete workflow instantly rather than piecing together information from multiple sources.
Documentation standards and compliance reminders benefit from the same approach. When staff need to verify they’ve included all required elements for medical necessity documentation, a shared checklist snippet provides the complete requirements: diagnosis codes demonstrating why the service was needed, documentation of evaluation before the service, notation of alternative treatments considered, explanation of why this service was appropriate, and any payer-specific documentation requirements. This systematic approach reduces omissions that lead to denials.
Training new hires becomes more effective when they have immediate access to standardized templates and workflows. Instead of trying to memorize everything during formal training, they learn where to find information and how to use tools that provide just-in-time access to what they need. The cognitive load shifts from memorization to understanding when and how to apply different requirements—a more sustainable and effective approach to building expertise.
Cross-training effectiveness improves dramatically when staff covering unfamiliar functions can access detailed workflows and requirements for those situations. The billing specialist who normally works commercial insurance can successfully handle a Medicare claim because they have access to Medicare-specific requirements, terminology, and processes. This capability reduces operational vulnerability when key staff are unavailable.
The knowledge preservation benefit becomes apparent during staff transitions. When experienced billing staff leave, they take institutional knowledge with them—those hard-won understandings of payer quirks, workarounds for system limitations, and mental models of what actually gets claims paid. When that knowledge exists in shared systems rather than only in individuals’ heads, the impact of turnover diminishes significantly. New staff can access the same information that took their predecessors years to accumulate.
Regulatory and coding updates present another area where centralized information distribution adds value. When ICD-10 codes update quarterly, CMS issues new rules, or payers change their policies, communicating those updates consistently across the team is challenging. Some staff miss emails, others don’t fully understand the implications, and months later you’re still correcting errors from outdated practices. Update distribution through snippet systems ensures everyone receives identical information immediately, with the context they need to implement changes correctly.
Consider creating snippet categories for different training and reference needs: onboarding sequences for new hires with progressive information release, payer-specific requirements organized by insurer, regulatory compliance reminders and checklists, authorization request templates with required information fields, appeal letter frameworks with payer-specific requirements, and troubleshooting guides for common scenarios. Staff access relevant information based on their situation rather than searching through comprehensive documentation to find what they need.
The standardization benefit extends beyond information access to actual claim submission. When staff use templates for appeal letters, authorization requests, or patient communication, the language stays consistent, required elements don’t get omitted, and quality remains high regardless of who’s working the case. This consistency improves both training effectiveness and operational performance.
Organizations that implement shared information systems report measurably better outcomes: faster time-to-productivity for new hires who access information rather than memorizing it, lower denial rates when staff consistently apply current requirements, improved cross-training effectiveness when covering unfamiliar functions, reduced supervisor interruptions as staff find answers independently, and better knowledge preservation during staff transitions.
The investment in centralized information tools represents a fraction of the cost of denied claims, productivity losses, and training inefficiencies. When you consider that each denied claim costs $25-50 to rework, preventing even a few denials monthly through better information access pays for the tools many times over.
Monitoring, Evaluating, and Refining Training Programs
Training programs need regular assessment and refinement to remain effective. Without systematic monitoring, you can’t determine if training actually improves performance, identify which curriculum components work well versus those that need adjustment, or justify continued investment in professional development.
Establish clear performance metrics that indicate training effectiveness. Track these key indicators: claim denial rate overall and by specific denial reason, clean claim rate showing percentage accepted on first submission, average days in accounts receivable, net collection rate measuring revenue actually collected, coding error rate from audits and reviews, time-to-independence for new hires, and staff retention rates. These operational metrics reveal whether training translates to better performance.
Create dashboards that visualize training impact on operational outcomes. Chart denial rates before and after training initiatives. Track how quickly new hires reach productivity milestones. Monitor whether denial patterns shift after targeted training interventions. When leadership can see clear connections between training investment and financial performance, continued support becomes straightforward.
Implement post-training assessments that validate learning before staff work independently. Design competency tests that mirror real work: claim coding exercises using actual scenarios, payer requirement application questions, compliance decision-making scenarios, and software proficiency demonstrations. Establish minimum competency scores that staff must achieve before handling production work without supervision. Staff who don’t meet standards receive additional training and support before working independently.
Conduct ongoing performance monitoring through regular work audits. Review a sample of each staff member’s work weekly or biweekly, providing feedback on accuracy, completeness, and adherence to requirements. Track individual performance metrics including claim accuracy rates, denial percentages, productivity levels, and quality scores. Use audit findings to identify both individual coaching needs and systematic training gaps that affect multiple staff members.
Analyze denial trends systematically to identify training needs. If authorization denials increase, that signals potential gaps in pre-certification processes. If medical necessity denials climb, documentation training might be required. If coding denials rise in specific areas, targeted coding refreshers are needed. Denial patterns reveal exactly where training should focus to prevent revenue loss.
Distinguish between individual performance issues and curriculum gaps. When one person consistently makes a particular type of error, that’s likely a coaching issue requiring individualized attention. When multiple staff make the same error, that suggests your training program didn’t adequately address that topic or the training didn’t stick. The distinction determines whether you need focused coaching or curriculum revision.
Gather feedback from multiple sources to assess training effectiveness. Survey trainees after training completion asking specific questions: Which topics were most/least clear? What additional practice would help? Were real-world applications adequately covered? What topics do you still feel uncertain about? Don’t just ask if they liked the training—ask if they can actually do the work better because of it.
Collect supervisor feedback on whether trained staff perform at expected levels. Ask supervisors: What additional training do new hires need? Which trained staff still require extensive supervision? What errors persist despite training? Where do staff demonstrate strong competency? Supervisor observations reveal gaps between training intentions and real-world performance.
Hold focus groups where staff discuss challenges they face and how training could better prepare them. The front-line billing team experiences daily realities that trainers might not fully appreciate. Their insights help refine training to address actual needs rather than theoretical requirements.
Review your training program comprehensively at least quarterly. Assess content currency given regulatory and payer changes, delivery method effectiveness based on learner feedback and outcomes, resource adequacy including time, tools, and trainer availability, and achievement of learning objectives and business goals. This systematic review keeps training aligned with evolving needs.
When you identify training gaps or ineffective approaches, act on that information promptly. If staff consistently struggle with a particular topic, revise how you teach it—try different examples, add more practice, provide better reference materials, or allocate more training time. If a delivery method isn’t working, experiment with alternatives. If assessments reveal knowledge gaps that training should have addressed, strengthen that curriculum component.
Track return on training investment quantitatively. Calculate the cost of developing and delivering training including staff time, materials, technology, and any external resources. Compare this investment to measurable improvements: denial reduction translated to revenue impact, faster time-to-productivity reducing coverage costs, improved retention decreasing turnover costs, and enhanced compliance reducing audit risk. Build the business case with actual data from your organization’s experience.
Consider implementing certification levels that recognize progressive competency development. Entry-level certification demonstrates basic competency in fundamental skills. Advanced certification reflects mastery of complex scenarios and payer-specific expertise. Specialist certification recognizes deep knowledge in particular areas like appeals or coding. This structured progression gives staff clear advancement paths and helps you identify who has demonstrated what capabilities.
Use technology to automate tracking where possible. Learning management systems record training completion and assessment scores automatically. Performance dashboards pull operational metrics without manual data gathering. Automated reporting saves time while ensuring consistent measurement.
The key principle is continuous improvement: monitor results, identify what works and what doesn’t, refine accordingly, measure again. Training programs should evolve based on evidence of effectiveness, not remain static because “that’s how we’ve always done it.” Organizations that systematically refine training based on outcome data achieve measurably better results than those that implement training once and never revisit it.
Ensuring Compliance and Ethical Standards in Training
Compliance training isn’t just about checking a legal requirement box—it’s about preventing serious financial and legal consequences while building a culture where ethical behavior is normal and expected. Healthcare billing compliance violations can result in substantial penalties, exclusion from federal programs, qui tam lawsuits under the False Claims Act, and criminal charges in egregious cases. Every billing staff member needs thorough understanding of compliance requirements and the ethical frameworks for navigating ambiguous situations.
Cover these essential regulations in your compliance training, ensuring staff understand both what the law requires and why it exists:
HIPAA privacy and security rules govern how billing staff handle protected health information. Staff must understand permissible uses of patient data for treatment, payment, and operations; the minimum necessary standard that limits access to what’s needed for each function; patient rights regarding their information; breach notification requirements; and security measures protecting electronic health information. Violations can result in substantial civil monetary penalties and criminal charges for willful violations.
The False Claims Act prohibits knowingly submitting false or fraudulent claims to federal healthcare programs. Help staff understand what constitutes a “false claim”: billing for services not actually rendered, upcoding by submitting codes for more expensive services than were provided, unbundling component services that should be billed with a comprehensive code, billing without adequate documentation of medical necessity, and duplicate billing for the same service. The law’s qui tam provisions allow private individuals to bring lawsuits on behalf of the government, creating substantial enforcement reach. Penalties include treble damages plus $11,000-22,000 per false claim.
The Anti-Kickback Statute prohibits offering, paying, soliciting, or receiving anything of value to induce referrals for services payable by federal healthcare programs. Billing staff should understand that kickback arrangements aren’t always obvious cash payments but can include excessive compensation for medical directorships, free or below-market rent, equipment provided below fair market value, and gifts or entertainment tied to referral expectations. Staff need to know how to recognize potentially problematic arrangements and escalate concerns.
Stark Law prohibits physicians from referring Medicare and Medicaid patients for designated health services to entities with which they have financial relationships unless an exception applies. While billing staff don’t typically structure these relationships, they need awareness that certain referral patterns might indicate Stark violations and should be reported to compliance leadership.
Medical necessity requirements demand that services be reasonable and necessary for diagnosis or treatment. Claims submitted without adequate documentation supporting medical necessity violate the False Claims Act even without fraudulent intent. Train staff to review documentation before submitting claims, recognize when documentation seems insufficient, and query providers when necessity isn’t clear from the record.
Create a compliance training program that meets legal requirements while genuinely preparing staff for real-world challenges. Federal requirements include training upon hire and annually thereafter, documentation of training completion with signed acknowledgments, coverage of relevant fraud and abuse laws, organization-specific compliance policies, and reporting mechanisms for suspected violations. Go beyond minimal compliance to build understanding of why these rules exist and how to apply them in practice.
Use scenario-based compliance training that presents realistic ethical dilemmas staff actually face: a physician pressures the billing team to code at the highest level supportable by documentation even when a lower level would be more accurate, a patient requests billing a covered service when they actually received a non-covered service, documentation is incomplete but the biller knows the procedure was definitely performed, a colleague mentions that a physician receives “consulting fees” from a supplier they frequently order from, or a supervisor suggests backdating documentation to meet filing deadlines. These scenarios develop judgment about when to push back, when to seek clarification, and when to escalate concerns.
Provide decision-making frameworks that help staff navigate gray areas: Is it legal? (Does it comply with laws and regulations?), Is it ethical? (Would I be comfortable if this was public knowledge?), Is it documented? (Can we demonstrate this decision was proper?), Is there precedent? (Have we done this before with compliance approval?), and Should I escalate? (Does this need leadership or compliance review?). These questions help staff think through ambiguous situations systematically.
Build a reporting culture where raising compliance concerns is encouraged and protected. Explain reporting mechanisms: who staff should contact with concerns, how anonymous reporting works if your organization has a hotline, that retaliation for good-faith reporting is prohibited, and what happens after a report is made. Make clear that asking questions about whether something is appropriate is always acceptable and demonstrates good judgment.
Address specific fraud and abuse patterns common in healthcare billing so staff can recognize them: upcoding through systematically selecting codes for more complex services than documentation supports, unbundling by billing component codes separately when a comprehensive code includes them, billing for services not rendered including phantom billing for no-shows, duplicate billing where the same service is billed multiple times, and medical necessity gaming where documentation is written to support billing rather than reflecting actual clinical judgment.
Teach staff to recognize red flags that might indicate compliance problems: pressure to code more aggressively, documentation patterns that seem designed for billing rather than care, unusual incentive structures tied to billing levels, resistance to questions about billing appropriateness, patterns of services that seem clinically inconsistent, and reluctance to discuss billing practices with auditors or regulators. Staff who notice these patterns need to know they should report concerns.
Document all compliance training meticulously. Maintain records showing training topics covered, dates completed, assessment results, and signed acknowledgments that staff received and understood the training. This documentation demonstrates good-faith compliance efforts and provides important protection if violations occur despite training. Courts and regulators look more favorably on organizations that demonstrate serious commitment to compliance.
Include leadership commitment to compliance in training materials. When executives and managers clearly communicate that compliance is non-negotiable and ethical conduct is expected, staff understand that raising concerns won’t harm their careers. This top-down commitment shapes organizational culture and establishes that revenue goals never justify compliance shortcuts.
Create an environment where compliance questions are routine and welcomed rather than viewed as obstacles. When staff ask “Is this appropriate?” or “How should we handle this situation?” treat those questions as demonstrations of good judgment. Organizations where compliance questions flow freely tend to catch and correct issues early before they become major problems.
The goal isn’t perfect knowledge of every compliance rule—that’s unrealistic given the complexity of healthcare regulations. The goal is developing judgment about when situations require extra scrutiny, building confidence to push back on inappropriate pressure, and creating clarity about reporting mechanisms for concerns. Staff who understand the serious consequences of compliance failures and feel supported in raising questions become your first line of defense against violations.
Incorporating Continuous Learning and Adaptation
Billing training can’t be a one-time event because the environment constantly changes. Payer policies update, coding systems evolve, regulations shift, and technology advances. Organizations that treat training as an ongoing process rather than a destination maintain better performance and adapt more successfully to change.
Build continuous learning into your operational rhythm through regular refresher training on foundational topics. Schedule quarterly sessions reviewing compliance requirements, common coding errors, documentation standards, and denial prevention strategies. These brief refreshers, perhaps 30-45 minutes during team meetings, keep critical knowledge current without requiring major time investment. Staff who completed initial training months or years ago benefit from periodic reinforcement of key concepts.
Create a systematic process for monitoring, communicating, and implementing regulatory changes. Designate someone to monitor authoritative update sources: CMS announcements and policy transmittals, AMA coding updates and guidance, major payer newsletters and policy bulletins, professional association communications, and specialty-specific regulatory information. When changes occur, quickly assess the impact on your operations, develop clear guidance for staff, update training materials and documentation, communicate changes to the team, and provide training on implementation.
Develop regulatory change communication templates that ensure consistent, complete information distribution. Each update announcement should include: what changed specifically, when the change becomes effective, why it matters to your organization, what actions staff must take, where to find detailed guidance, and who to contact with questions. This structured approach prevents the confusion that occurs when change communications are ad-hoc and incomplete.
Implement just-in-time learning resources that staff access exactly when needed. Create brief video tutorials for software features, one-page job aids for new procedures, FAQ documents addressing common questions, quick-reference guides for policy changes, and searchable knowledge bases for troubleshooting. Staff facing unfamiliar situations need immediate access to guidance, not to wait for the next scheduled training session.
When major payer policy changes occur—authorization requirement revisions, billing rule updates, or documentation standard changes—create focused update modules that staff complete promptly. These “flash training” sessions keep your team current without requiring comprehensive curriculum revision. The modular approach you built earlier makes these targeted updates straightforward.
Encourage staff participation in external learning opportunities that broaden their expertise: webinars from payers explaining policy updates, professional association courses on specialized topics, specialty-specific billing workshops, and coding certification continuing education. Provide time and support for staff to pursue these development opportunities. The knowledge they gain benefits your organization while demonstrating your investment in their professional growth.
Share relevant industry information with your team regularly. When authoritative sources publish useful articles, case studies, or guidance, distribute them to staff with context about why the information matters. Create brief summaries of lengthy regulatory documents so staff understand key points without reading 50-page policy manuals. Position yourself as the curator helping staff stay informed without overwhelming them.
Hold regular team meetings where staff discuss challenging scenarios, share problem-solving approaches, and learn from each other. The billing specialist who found a better way to research payer policies shares that technique. The staff member who successfully appealed a complex denial explains their approach. Peer learning leverages the collective expertise within your team.
Recognize and reward staff who demonstrate commitment to continuous learning. Acknowledge completion of certifications, participation in training programs, and contribution to team knowledge sharing. This recognition reinforces that professional development is valued and expected.
Stay current with technology advances affecting billing: updates to your EHR and practice management systems, new claim scrubbing capabilities, AI-assisted coding tools, predictive analytics for denial prevention, and automation possibilities for routine tasks. Provide training on new technology features as they become available. Help staff understand not just how to use tools but how they impact workflows and decision-making.
Create learning opportunities from your own performance data. When denial trends shift, conduct root cause analysis and share findings with the team. When successful appeals provide insights into payer interpretation, document those lessons. When audit findings reveal documentation gaps, use them as teaching opportunities. Your organization’s actual experience provides highly relevant training content.
Build a culture where continuous learning is normal and expected rather than extra or optional. Frame ongoing training as part of the job, not additional burden. Protect time for professional development. Support certification pursuits. Celebrate knowledge advancement. Organizations that embed continuous learning into their culture adapt more successfully to the constant change characterizing healthcare billing.
The investment in continuous learning pays off through better adaptation to change, improved staff capabilities over time, enhanced job satisfaction and engagement, and reduced vulnerability to new denial patterns or compliance risks. When your team expects to keep learning and has mechanisms supporting that ongoing development, change becomes manageable rather than overwhelming.

Engaging Leadership and Securing Organizational Support
Training programs succeed or fail based on organizational commitment. Without leadership support, training gets deprioritized when operational demands increase, resources get diverted to other priorities, and staff perceive training as optional rather than essential. Building strong executive sponsorship creates the foundation for training program success.
Begin by demonstrating how training investment directly supports organizational strategic priorities. If leadership focuses on improving financial performance, show how training reduces denial rates and accelerates cash flow. If patient satisfaction is a priority, demonstrate how better-trained billing staff resolve patient issues more effectively and professionally. If compliance risk is a concern, highlight how comprehensive training reduces audit exposure. Frame training in terms that resonate with each stakeholder’s specific priorities rather than generic arguments about professional development.
Build your business case with concrete financial projections. Calculate the current cost of billing errors and denials: number of denials monthly, average cost to rework each denial ($25-50 is a reasonable estimate), and indirect costs from cash flow delays. Project training impact based on realistic improvement targets: reducing denial rate from 10% to 7% might be achievable within 6 months. Translate those improvements to revenue impact: if you submit 1,000 claims monthly with a 10% denial rate and $100 average claim value, a 3% reduction in denials saves $3,000 monthly or $36,000 annually just in claims that get paid earlier with less rework.
Compare training costs to the value of improvements. If developing and delivering a comprehensive training program costs $25,000 in staff time, materials, and resources but produces $36,000 in annual measurable savings, the ROI is clear. Factor in additional benefits that are harder to quantify but nonetheless real: improved staff retention reducing turnover costs, enhanced compliance reducing audit risk, and better staff morale improving productivity.
Calculate the cost of inadequate training through staff turnover. Replacing a billing specialist costs between $15,000-25,000 when you include recruitment, onboarding, and the 3-6 months of reduced productivity before new hires reach full competency. If effective training and professional development improves retention by even 10-15%, the savings quickly exceed training costs.
Secure visible executive sponsorship where senior leaders champion training initiatives. Have executives communicate the importance of training to staff, participate in program launches or key training sessions, review training metrics and outcomes regularly, and allocate necessary resources despite competing demands. When staff see that leadership treats training as a priority, they take it more seriously.
Create accountability structures that ensure training happens consistently. Include training-related goals in manager performance evaluations: completing scheduled staff training, achieving team competency standards, and improving relevant operational metrics. When managers know their performance reviews include training outcomes, they protect training time and ensure quality delivery.
Establish regular reporting cadences where training outcomes are reviewed alongside other organizational performance indicators. Present denial rate trends and connect improvements to training initiatives. Share time-to-productivity data showing faster onboarding from enhanced training. Report staff feedback on training value and professional development satisfaction. These regular updates keep training visible and demonstrate ongoing value.
Address resource allocation explicitly with leadership. Training requires protected time where staff aren’t pulled for operational work, budget for materials, technology, and external resources, dedicated training space if conducting in-person sessions, and potentially dedicated training staff if your program is substantial. Secure commitment to these resources upfront rather than fighting for them repeatedly as training needs arise.
Help leadership understand that protecting training time pays off operationally. The hours invested in training return multiples in reduced errors, lower denial rates, and faster problem resolution. Cutting training to maximize immediate productivity might feel efficient but creates long-term performance problems that cost far more than the time saved.
Communicate training value to staff so they understand why it matters. Help them see how training reduces job stress by building competence and confidence, creates advancement opportunities through skill development, improves daily workflow by reducing errors and rework, and demonstrates the organization’s investment in their success. Staff who understand training benefits engage more seriously.
Celebrate training achievements publicly. Recognize staff who complete certifications, achieve competency milestones, or contribute to team knowledge sharing. These celebrations reinforce that professional development is valued and create positive peer pressure for others to engage with training opportunities.
Share success stories that illustrate training impact. When denial rates drop after targeted training, share that success. When a newly trained employee successfully handles a complex scenario, acknowledge it. When cross-training enables seamless coverage during absences, highlight that benefit. These stories make abstract training value concrete and relatable.
Address concerns about training costs and time investment honestly. Yes, training requires resources and time away from immediate operational work. But the alternative—inadequately trained staff making costly errors—is far more expensive. Frame the choice accurately: you can invest in training proactively or pay for errors and inefficiency reactively. The first approach costs less and produces better outcomes.
Build a coalition of training supporters across the organization. Engage supervisors and managers who see daily training value, involve finance leaders who can quantify the business case, enlist compliance officers who appreciate risk reduction, and recruit high-performing staff who can advocate for professional development. This broad base of support makes training initiatives more resilient.
The fundamental principle is demonstrating value consistently through measurable outcomes. When leadership sees that training investment produces concrete business results—improved financial performance, reduced risk, better retention, enhanced quality—continued support becomes straightforward. Training programs that can’t demonstrate value struggle to maintain support; those that show clear ROI find resources and commitment readily available.
Transform Your Billing Team Training Today
Join healthcare organizations that are reducing training time, preventing denials, and preserving critical billing knowledge with TextExpander. Give your team instant access to payer requirements, authorization workflows, and billing templates that reduce errors and accelerate productivity.
Frequently Asked Questions
What topics should a medical billing training program cover to be effective?
An effective medical billing training program must cover the complete billing cycle from registration through collections, medical coding with ICD-10, CPT, and HCPCS, payer-specific requirements for your major insurers, compliance regulations including HIPAA and the False Claims Act, denial prevention and resolution, authorization processes, and documentation standards. Beyond these fundamentals, tailor your program to your organization’s specific payer mix, specialties, and common error patterns. Include extensive hands-on practice with your actual billing software and realistic claim scenarios that represent your case mix. The combination of knowledge and practical application makes training stick and translates to better performance.
How long does it take to train new medical billing staff?
Training duration varies based on prior experience, position complexity, and your organization’s standards. Completely new billing staff typically require 2-3 months of intensive training plus another 3-6 months to reach full productivity. Staff with prior billing experience may need 4-8 weeks of organization-specific training to learn your systems, payers, and workflows. You can shorten this timeline with structured programs that include clear competency standards, effective mentorship, and tools that provide quick access to reference information staff need. Organizations investing in comprehensive training see faster time-to-productivity and substantially lower error rates compared to those using sink-or-swim approaches.
How do you keep billing staff updated on constantly changing payer requirements?
Maintaining current knowledge requires a systematic approach: designate someone to monitor payer policy updates from bulletins, newsletters, and provider portals; establish communication channels for rapid information distribution when policies change; update training materials and reference resources immediately when policies change; provide brief refresher training on significant changes; create centralized resources where staff can access current payer requirements; and implement regular team meetings where policy changes are discussed. Many organizations find success using snippet libraries or knowledge bases that can be updated once and accessed by all staff, ensuring consistency. The key is treating regulatory compliance as an ongoing process rather than a one-time training event.
What’s the best way to train remote or offshore billing teams?
Training remote teams requires adapting delivery methods while maintaining content quality. Use recorded training sessions that remote staff can access on-demand regardless of time zones, conduct live virtual training via video conferencing for interactive content, provide detailed documentation with screenshots and workflows, establish virtual office hours for questions and coaching, and use screen-sharing tools for software training and troubleshooting. Ensure remote staff have identical access to knowledge bases, snippet libraries, and reference materials that on-site staff use. Consider time zone differences when scheduling live sessions. Create asynchronous learning options where possible. Address any compliance or security requirements for remote staff access to training materials and billing systems. The goal is equivalent training quality regardless of location.
How can I reduce billing errors during the training period?
Implement graduated responsibility where trainees work simpler claims before advancing to complex cases, require supervisor review of trainee work until they demonstrate competency, use claim scrubbing software to catch errors before submission, provide trainees with detailed checklists and reference materials for common scenarios, and establish clear escalation processes for questions. Create an environment where trainees feel comfortable asking questions rather than guessing. Consider dual-review processes during training where mentor and trainee review claims together, using errors as learning opportunities with constructive feedback rather than punitive responses. Track common error types and provide targeted remediation training. The investment in oversight during training prevents costly errors and builds solid habits that persist after trainees work independently.
How do I measure if my billing training program is effective?
Measure training effectiveness through multiple lenses: pre- and post-training knowledge assessments showing what staff learned, time-to-independence for new hires compared to historical averages, operational metrics including denial rate, clean claim rate, and days in AR before and after training, trainee and supervisor satisfaction surveys, and staff retention rates. Compare performance metrics between well-trained staff and those who received minimal training. Track how quickly staff adapt to payer policy changes after receiving update training. Monitor whether common errors decrease following targeted training interventions. Review whether trained staff require less supervisor intervention and work more independently. Effective training should demonstrate measurable improvement in accuracy, productivity, compliance, and job satisfaction—all translating to better financial performance.
What are key strategies to reduce claim denials through training?
Focus training on your organization’s most common denial reasons: improper coding and code linkage, missing or incorrect authorizations, insufficient documentation supporting medical necessity, registration errors including incorrect insurance information or missing referrals, untimely filing, and payer-specific requirement violations. Teach staff to prevent denials proactively through accurate upfront processes rather than focusing solely on appeals. Provide extensive training on payer-specific requirements since each insurer has unique rules causing denials. Include training on researching denial reasons and determining root causes. Implement quality checks at each billing cycle stage. Use real denial examples from your organization to make training relevant and demonstrate consequences of errors. The most effective approach addresses denial prevention systematically across the entire billing cycle rather than just training staff to write appeals.
How do I cross-train billing staff when everyone is already busy?
Cross-training requires strategic planning and leadership commitment to long-term capability over short-term productivity. Start by identifying critical functions needing coverage redundancy. Implement gradual cross-training where staff learn adjacent functions over time rather than all at once. Use slower periods or schedule specific cross-training time into weekly work plans. Consider job rotation where staff temporarily work in different functions. Create comprehensive documentation and reference materials supporting quick learning when coverage is needed. Use shadowing opportunities where staff observe others during regular work. Recognize that investing time in cross-training pays off through reduced vulnerability during absences, turnover, or volume surges. Frame cross-training as career development benefiting staff by expanding their skills and advancement opportunities. The operational resilience and flexibility you gain justify the time investment.
What compliance training is legally required for billing staff?
Billing staff require training on several federal regulations. HIPAA privacy and security training is mandatory upon hire and annually thereafter, covering permissible uses of protected health information and breach reporting. Organizations billing federal programs (Medicare/Medicaid) must provide fraud, waste, and abuse training covering the False Claims Act, Anti-Kickback Statute, and Stark Law. All compliance training must be documented with completion records and signed acknowledgments. Beyond legal minimums, best practices include training on medical necessity documentation standards, proper coding and billing practices, organizational compliance policies and procedures, and reporting mechanisms for suspected violations. Establish a culture where compliance is everyone’s responsibility, not just a checkbox exercise. The goal is building judgment about when situations require extra scrutiny and creating confidence to push back on inappropriate pressure.
How can productivity tools help standardize billing training?
Productivity tools addressing one of billing’s biggest challenges—managing complex, constantly changing information consistently across teams. They enable instant distribution of payer requirement updates, ensure all staff access identical current information, provide new hires immediate access to templates and reference materials, support cross-training by giving staff quick access to unfamiliar payer requirements, and preserve institutional knowledge when experienced staff leave. Rather than staff maintaining personal notes or relying on memory, shared snippet libraries create a single source of truth for payer requirements, authorization processes, compliance reminders, and billing workflows. When policies change, updating centralized snippets ensures everyone immediately has current information, preventing outdated practices that lead to denials. This approach accelerates training effectiveness, reduces errors, and maintains consistency across your entire billing team.
Supporting Your Training Success
Building effective medical billing training programs requires significant investment in curriculum development, delivery systems, and ongoing refinement. The complexity of healthcare billing, combined with constant regulatory changes and staffing challenges, makes training one of your most important operational priorities.
The organizations seeing the best results from training investment share common characteristics: systematic approach to needs assessment and curriculum development, executive commitment to protecting training time and resources, measurement systems proving training impact on operational performance, continuous refinement based on outcomes and feedback, and tools supporting consistent information access and knowledge preservation.
Your training program doesn’t need to be perfect from the start—it needs to be good enough to improve performance measurably, then continuously refined based on results. Start with your most critical training needs, implement systematically, measure outcomes, and build from there. The improvement in denial rates, staff productivity, retention, and financial performance will justify continued investment.
The 43% staffing crisis facing healthcare billing departments won’t resolve itself. Organizations that invest in making their teams more effective through comprehensive training will outperform those hoping to solve staffing shortages through recruitment alone. When you can’t hire enough qualified people, making the people you have more capable becomes essential.

