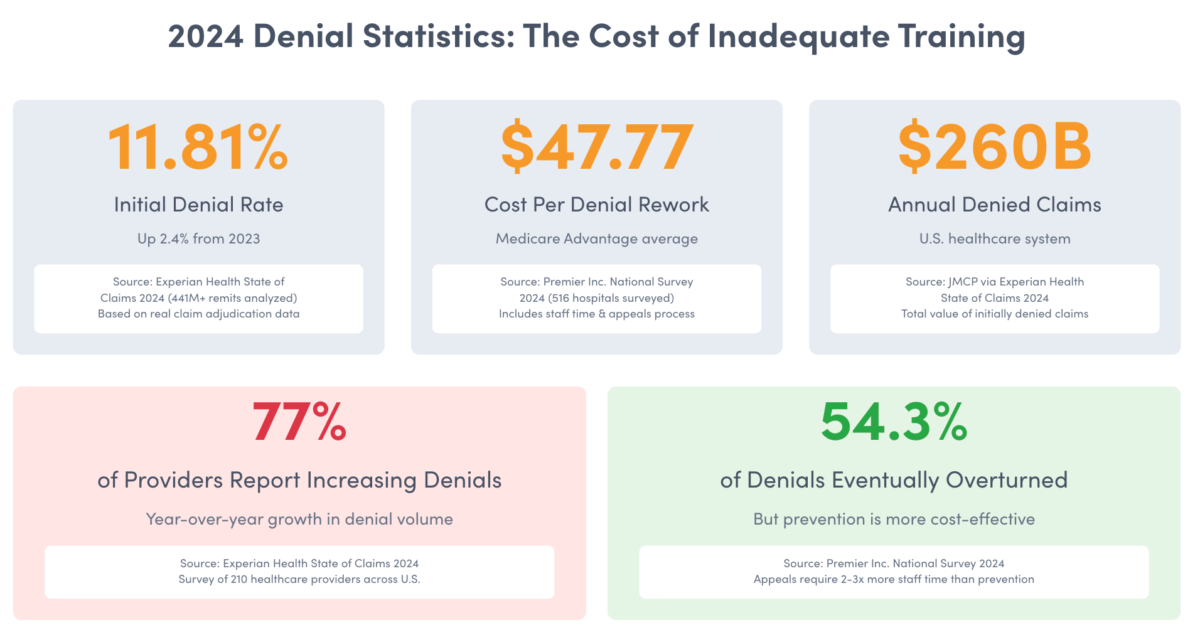
Claim denial rates hit 11.81% in 2024, according to Experian Health’s State of Claims report. That’s not just a statistic. It’s real revenue walking out the door every single day. Behind every denied claim sits undertrained staff who don’t know what they don’t know.
The financial impact is staggering. Healthcare organizations lose an estimated $260 billion annually to denied claims, according to The Journal of Managed Care & Specialty Pharmacy. Each denied claim costs between $25 and $50 to rework, and many denied claims are never resubmitted, leading to permanent revenue loss.
But here’s what the numbers don’t show: the stress on your existing staff who have to pick up the slack, the turnover that comes from throwing new hires into complex workflows without proper training, and the compounding effect when errors cascade through your entire revenue cycle.
You can’t afford to wait six months for new hires to “figure it out.” Revenue cycle management training needs to be systematic, comprehensive, and fast. This guide shows you exactly how to build an RCM training program that gets new staff productive in weeks, not months, while setting them up for long-term success.

Free: Medical Billing Snippets
Download 27 TextExpander Snippets to help make your medical billing team more accurate and more consistent. Save time and reduce denied claims.
Why Revenue Cycle Management Training Fails (And What to Do About It)
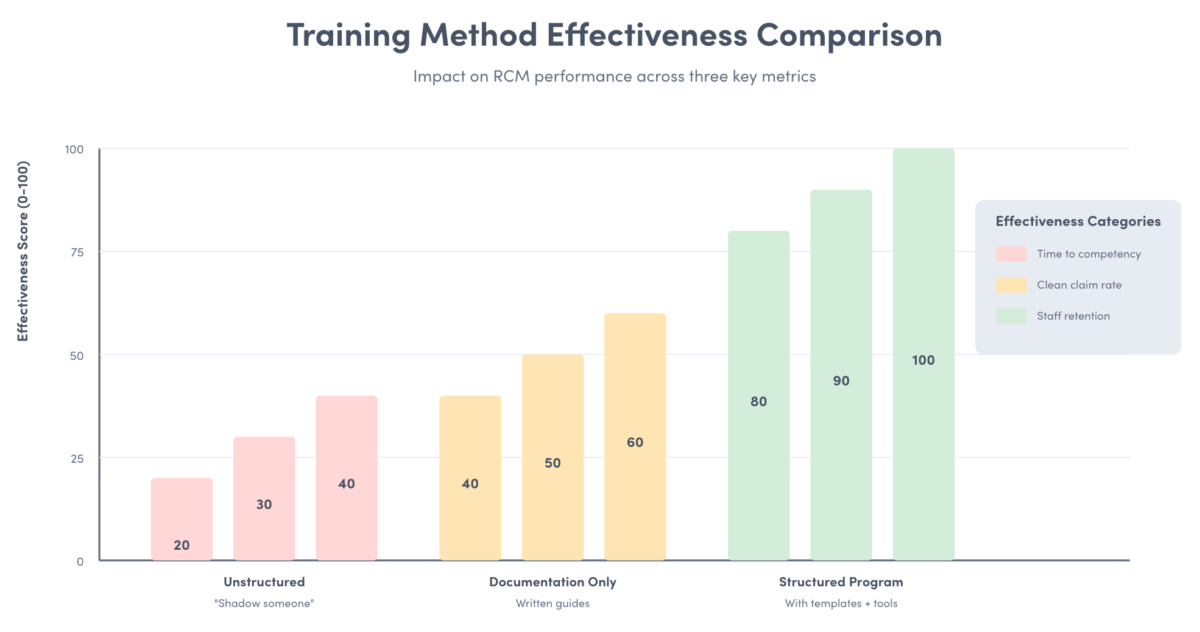
Most healthcare organizations approach RCM training backwards. They hand new hires a massive policy manual, have them shadow someone for a few days, then expect them to process claims independently. This approach fails because it treats training as information transfer rather than skill development.
The problem compounds when the person doing the training has developed bad habits over years of work. Those shortcuts and workarounds get passed to new hires, creating a cycle of inefficiency that’s hard to break.
Effective revenue cycle management training requires three elements: structured progression from basics to complexity, hands-on practice with real-world scenarios, and continuous feedback that catches errors before they become habits. Medical billing training works the same way. You can’t skip the fundamentals just because you’re in a hurry to fill staffing gaps.
Here’s what works: Start with the revenue cycle’s financial logic. Help new hires understand why each step matters to the bottom line. When someone grasps that improper documentation costs the organization thousands of dollars per claim, they approach their work differently than if they’re just “filling out forms.
Training should mirror real work rhythms. Don’t spend three weeks in a classroom before touching actual claims. Instead, alternate between concept introduction, supervised practice, and independent work with spot-checks. This approach builds confidence while catching mistakes early.
The biggest training mistake is treating everyone the same. Someone with medical coding experience needs different training than a registrar moving into billing. Customize your program based on prior knowledge and role requirements.
Understanding Revenue Cycle Management Fundamentals
Revenue cycle management is the end-to-end administrative process of patient care from scheduling through final payment collection. It’s how healthcare organizations capture revenue they’ve earned by providing care. The cycle starts before a patient walks through the door and extends months after treatment ends.
The revenue cycle encompasses eight core phases: patient registration and insurance eligibility verification, charge capture and coding, claim submission, payment posting, denial management, patient billing, collections, and reporting and analysis. Each phase depends on accuracy from the previous phase. Errors compound as claims move through the cycle.
New staff need to understand the financial stakes. Healthcare operates on margins between 1% and 4%, according to industry benchmarks. When claims don’t get paid correctly the first time, that slim margin evaporates fast. Documentation failures don’t just delay payment. They directly reduce revenue.
The revenue cycle connects clinical care to financial outcomes. When a provider documents a patient visit, that documentation must support the codes billed. When a registrar collects insurance information, that data determines whether claims get paid. Every role in the revenue cycle affects whether the organization captures revenue or leaves money on the table.
Train new hires on the relationship between clinical documentation and claim payment. A provider’s notes must demonstrate medical necessity for billed services. Missing a single element, like documenting the patient’s symptoms or the reasoning behind a diagnostic test, can trigger automatic denials that require costly appeals.
Insurance verification happens before care but affects everything downstream. Staff who skip thorough eligibility checks create problems weeks later when claims get denied for coverage issues that could have been caught upfront. This verification step isn’t bureaucratic box-checking. It’s revenue protection.
Speed Up RCM Training While Reducing Documentation Errors
Give new hires instant access to pre-approved claim templates, denial management scripts, and payer-specific requirements. TextExpander’s healthcare templates ensure consistency from day one.
Key Performance Metrics Every New Hire Must Master
New staff can’t improve what they don’t measure. Training should include how to track and interpret core RCM metrics that directly indicate their performance and impact on organizational health.
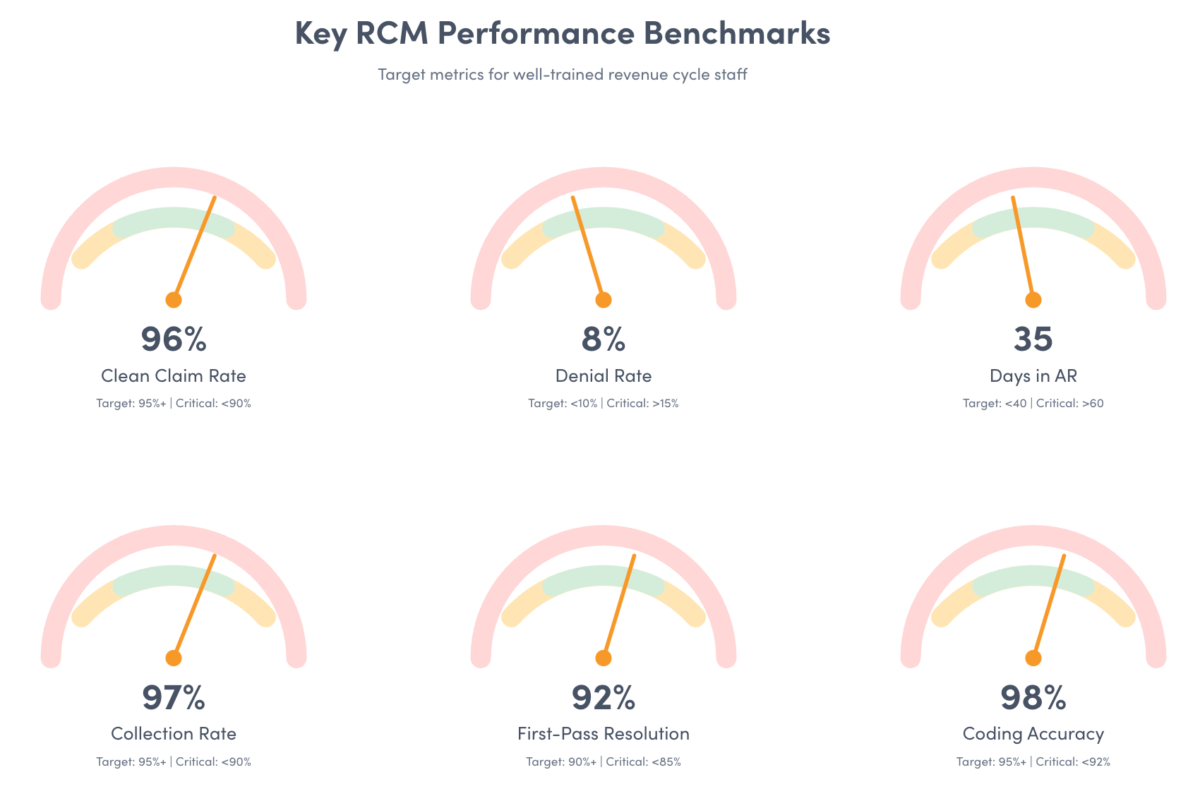
Clean claim rate measures the percentage of claims paid on first submission without additional information or corrections. Benchmark targets exceed 95%. When your clean claim rate drops below this threshold, you’re spending too much time on rework instead of processing new claims. New hires should understand that every percentage point below 95% represents thousands of dollars in delayed revenue and increased administrative costs.
Days in accounts receivable (AR) measures how long it takes to collect payment after services are provided. Healthy practices maintain AR days below 40 for commercial insurance and below 30 for Medicare. Rising AR days signal bottlenecks somewhere in your revenue cycle: claims sitting unworked, denied claims not appealed promptly, or patient balances not followed up.
First-pass acceptance rate tracks claims accepted by payers on first submission. This metric differs from clean claim rate by measuring payer acceptance rather than internal quality standards. According to Premier Inc.’s 2024 survey, nearly 15% of all claims submitted to private payers are initially denied, meaning first-pass acceptance rates average around 85%.
Denial rate measures the percentage of claims rejected by payers. Experian Health’s 2024 State of Claims report found that 77% of providers report increasing denial rates, with 38% of organizations experiencing denials on at least one in ten claims. New hires should learn to categorize denials by reason: coding errors, authorization issues, eligibility problems, or medical necessity disputes.
Collection rate calculates the percentage of collectible revenue actually collected. This metric accounts for contractual adjustments and bad debt write-offs. Strong collection rates exceed 98% for insurance and 70% for patient responsibility. Lower rates indicate problems with denial management, patient communication about balances, or payment plan offerings.
Average reimbursement rate compares actual payments received to charges submitted. This metric helps identify underpayments and payer contract compliance issues. New staff should learn to spot patterns where certain payers consistently reimburse below contracted rates.
Net collection rate measures payments received divided by payments that should have been received after contractual adjustments. This ratio reveals your revenue cycle’s overall effectiveness. Rates below 95% suggest significant revenue leakage through write-offs, denials, or underpayments.
Train new hires to review these metrics weekly during their first three months. Have them track their individual performance alongside team benchmarks. When someone sees their clean claim rate improving from 88% to 94% over four weeks, they understand the tangible impact of improved accuracy.
Mastering Patient Registration and Insurance Verification
Patient registration sets the foundation for everything downstream in the revenue cycle. Errors at this stage compound as claims move through the system, creating denials that could have been prevented with accurate upfront data collection.
Registration staff collect five critical data categories: patient demographics (name, date of birth, address, contact information), insurance information (member ID, group number, policy dates, primary and secondary coverage), guarantor information (responsible party for patient balances), emergency contacts, and consent forms (HIPAA, treatment authorization, financial responsibility).
The accuracy requirement is absolute. A transposed digit in a member ID number triggers claim rejections. A wrong date of birth creates eligibility mismatches. Missing or incorrect insurance group numbers prevent claims from routing properly. New staff must understand that registration isn’t data entry. It’s revenue protection.
Insurance verification confirms coverage before services are rendered. Real-time eligibility checks through payer portals reveal: whether coverage is active on the date of service, patient deductible amounts and what’s been met, copayment and coinsurance responsibilities, coverage limitations and exclusions, and prior authorization requirements.
Train new registrars to verify insurance for every encounter, even established patients. Coverage changes without notice. Patients switch jobs, lose coverage, or add secondary insurance. Assumptions about coverage create claim denials weeks later when treatment has already been provided.
Prior authorization requirements vary by payer, procedure, and diagnosis. New staff need to know which services require authorization and how to check authorization status. Services rendered without required authorization face immediate denials that are difficult to overturn. The cost of a denied $15,000 procedure because someone didn’t verify authorization falls directly on the organization.
Healthcare communication tools help registration staff maintain accuracy while working efficiently. When everyone uses the same verification scripts and documentation templates, you reduce variability and catch errors before claims are submitted.
Demographic verification matters more than most new staff realize. Middle initials, name suffixes (Jr., Sr., III), and hyphenated names must match insurance records exactly. Payers reject claims for name mismatches even when other identifiers are correct. Train staff to collect information exactly as it appears on insurance cards rather than assuming how names should be spelled.
Address accuracy affects patient collections. If statements go to the wrong address, patient balances go uncollected and eventually get written off. Verify addresses at every encounter and ask patients directly if anything has changed since their last visit.
Building Medical Coding and Documentation Excellence
Medical coding translates clinical documentation into standardized codes that payers use to determine coverage and payment. New staff need to understand three primary code sets: ICD-10-CM for diagnoses, CPT for procedures and services, and HCPCS for supplies and specialized services.
ICD-10-CM (International Classification of Diseases, 10th Revision, Clinical Modification) codes describe what was wrong with the patient, their diagnoses, symptoms, and conditions. These codes establish medical necessity for services provided. When documentation supports a diagnosis of “Type 2 diabetes mellitus with diabetic chronic kidney disease” rather than just “diabetes,” the specificity supports higher reimbursement and demonstrates appropriate care complexity.
Specificity in diagnosis coding directly affects payment. Payers require documentation to support the level of service billed. Vague documentation like “chest pain” doesn’t support the same evaluation and management level as “acute chest pain with radiation to left arm, patient with history of hypertension and hyperlipidemia, EKG changes consistent with ischemia.” Train new staff to recognize when documentation lacks sufficient detail to support billed codes.
CPT (Current Procedural Terminology) codes describe what was done for the patient, the services, procedures, and treatments provided. These codes must be supported by documentation that describes the work performed, time spent, medical decision-making complexity, and resources utilized.
Evaluation and management (E/M) codes require specific documentation elements. The 2021 E/M guideline changes simplified requirements but documentation must still support the chosen service level. New coders need to understand how medical decision-making complexity, time spent, and documentation requirements determine appropriate E/M codes.
HCPCS (Healthcare Common Procedure Coding System) codes cover supplies, equipment, and services not included in CPT. These codes become particularly important for practices providing durable medical equipment, certain drugs, or specialized services. Train new staff to recognize when HCPCS codes apply instead of or in addition to CPT codes.
Coding accuracy requires understanding the relationship between diagnosis and procedure codes. Diagnosis codes must support the medical necessity of procedure codes billed. When a patient receives an extensive diagnostic workup, the diagnosis codes must justify why that level of investigation was medically appropriate. Missing this connection creates medical necessity denials.
Documentation requirements vary by payer. Medicare has different documentation standards than commercial insurance, and each commercial payer may have additional requirements. New staff should learn payer-specific documentation requirements for common procedures in your specialty.
Medical billing compliance depends on accurate coding that reflects services actually provided. Overcoding generates compliance risk and audit exposure. Undercoding leaves revenue on the table. Both represent failure to document and code appropriately.
Code updates happen annually. ICD-10-CM and CPT codes change every October. New codes are added, old codes are deleted, and descriptions are modified. Training must include how to stay current with coding changes and where to find updated guidance.
Effective Claims Submission and Management Processes
Claims submission converts the work of registration, documentation, and coding into a request for payment. Electronic claims submission has become the industry standard, offering faster processing and immediate feedback on formatting errors.
Claims scrubbing happens before submission to payers. Automated scrubbing software checks for common errors: invalid diagnosis-procedure code combinations, missing required fields, duplicate claim submissions, authorization number mismatches, and coverage date inconsistencies. New staff should learn to review scrubbing reports and correct errors before transmission.
Clean claims pass scrubbing and reach the payer without requiring additional information. The claim contains all required data elements: patient and insurance identification, provider and facility information, dates of service, procedure and diagnosis codes, charges for services rendered, and any required authorization numbers.
Claim submission timing matters. Most payers impose filing deadlines, with claims submitted after the deadline facing automatic denial. Commercial payers offer filing windows between 90 and 180 days from date of service. Medicare requires claims within one year. Training should emphasize submitting clean claims promptly rather than holding batches.
Electronic remittance advice (ERA) provides payer responses to submitted claims. New staff need to understand ERA formats and how to read explanation of payment (EOP) codes. These codes indicate whether claims were paid, denied, or adjusted, along with the specific reason for each action.
Claim status tracking prevents revenue leakage. Claims can get lost in transmission, sit in payer queues without processing, or require additional information that staff miss. Implement systematic follow-up: check claim status at 7 days for any payer acknowledgment, at 14 days for claims not yet processed, at 21 days for claims with status inquiries, and at 30 days for claims without payment or denial.
Electronic claim submission reduces errors compared to paper claims. Electronic formats enforce required fields, validate code combinations before transmission, and provide immediate feedback on formatting issues. Most payers reject paper claims or assess processing penalties that reduce reimbursement.
Clearinghouse submission offers an intermediary layer that scrubs claims before forwarding to payers. Clearinghouses identify errors that would trigger payer denials, provide standardized formatting across multiple payers, and offer detailed reporting on claim status and denials. New staff should learn your clearinghouse’s reporting tools and how to interpret rejection reports.
Timely filing awareness prevents unnecessary denials. Every payer has filing deadlines, and these deadlines are firm. Claims submitted even one day past deadline face automatic denial regardless of how clean the claim is. Train new staff to prioritize older claims approaching filing deadlines over newer claims with more time remaining.
Denial Management and Appeals Strategy
Denial management recovers revenue from rejected claims and identifies patterns to prevent future denials. Premier Inc.’s 2024 survey found that more than half of denied claims (54.3%) are eventually overturned on appeal, but at an average cost of $47.77 per Medicare Advantage claim.
Denial categorization helps identify root causes. Group denials into five main categories: technical denials from registration or eligibility errors, coding denials from incorrect or unsupported codes, authorization denials from missing or expired authorizations, medical necessity denials from insufficient documentation, and timely filing denials from late submissions.
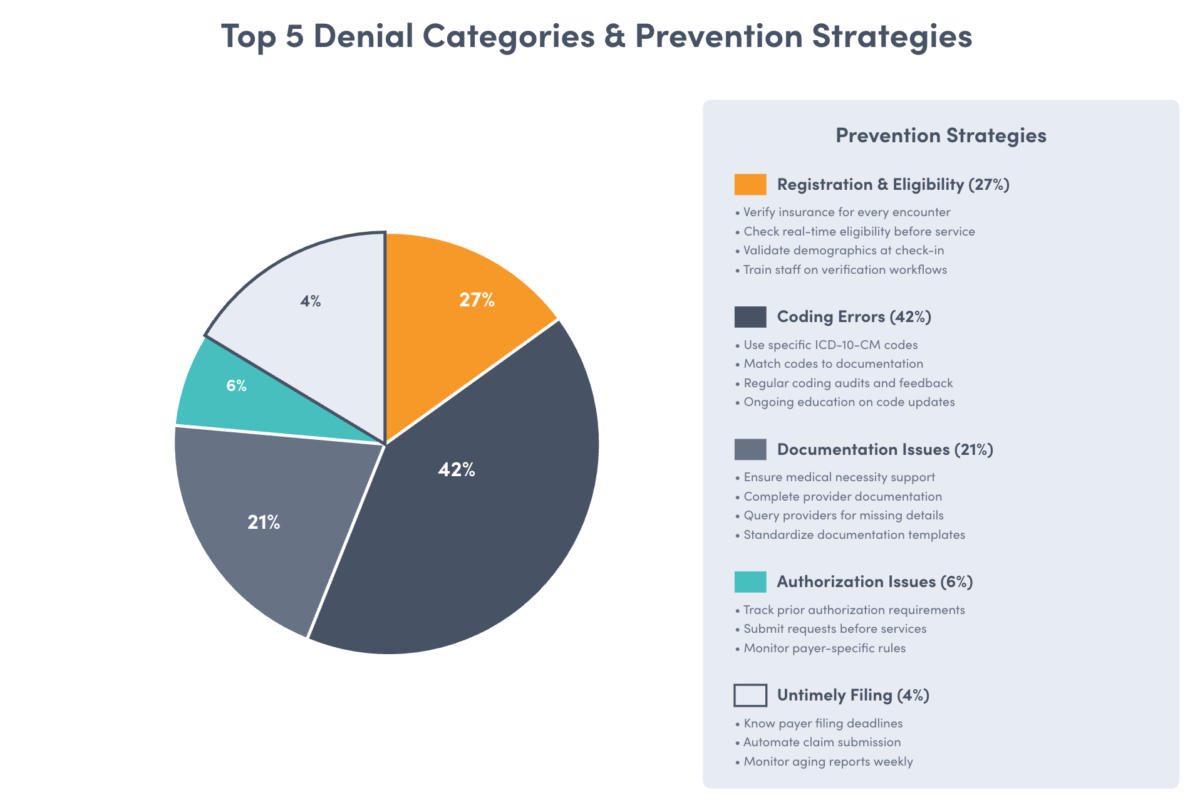
Technical denials often stem from registration errors: wrong patient ID numbers, inactive coverage dates, or demographic mismatches. These denials are preventable through proper verification at check-in. When technical denials cluster around certain staff members or registration desks, targeted retraining resolves the pattern.
Coding denials indicate mismatches between services billed and documentation provided. Common coding denial reasons include unbundling procedures that should be reported together, using outdated or invalid codes, billing mutually exclusive procedures, and lacking specificity in diagnosis codes. These denials require understanding the specific payer’s coding policies and ensuring documentation supports billed codes.
Authorization denials happen when services require prior approval but were rendered without obtaining authorization. These are among the most frustrating denials because the service has already been provided and some payers refuse payment regardless of medical necessity. Prevention requires robust authorization workflows that catch requirements before scheduling.
Medical necessity denials occur when payers determine that documentation doesn’t support the service provided. These denials require appeals with additional clinical documentation demonstrating why the service was appropriate. Success rates on medical necessity appeals vary widely by payer and service type.
Timely filing denials are final. Once a payer’s filing deadline passes, there’s no appeal except in rare circumstances where the delay was the payer’s fault. These denials represent permanent revenue loss and emphasize why claim submission can’t wait.
Appeal processes vary by payer but follow general patterns. First-level appeals typically involve submitting additional documentation or clarification letters. Second-level appeals may include peer-to-peer clinical reviews. Third-level appeals might involve external review by independent organizations. The Commonwealth Fund reports that insurers approved at least some form of care for about half of those who appealed denials.
Train new staff on your organization’s appeal prioritization criteria. Not all denials are worth appealing. When appeal costs exceed potential recovery, the denial should be written off. Focus appeal efforts on high-dollar denials, pattern denials that indicate systematic problems, and denials where you have strong supporting documentation.
Denial trend analysis prevents future revenue loss. Weekly or monthly reporting should show denial rates by payer, denial reason, service type, and provider. When one payer starts denying a procedure they previously paid, investigate immediately. Payer policies change and staff need to adapt quickly.
Documentation improvement directly reduces denials. When medical necessity denials cluster around specific procedure codes, work with providers to enhance documentation for those services. When authorization denials spike, examine your authorization tracking process to identify where requirements are being missed.
Leveraging Technology and Automation in RCM
Technology doesn’t replace human judgment in revenue cycle management. It amplifies the effectiveness of well-trained staff. Automation handles repetitive tasks, allowing staff to focus on complex problem-solving and exception handling.
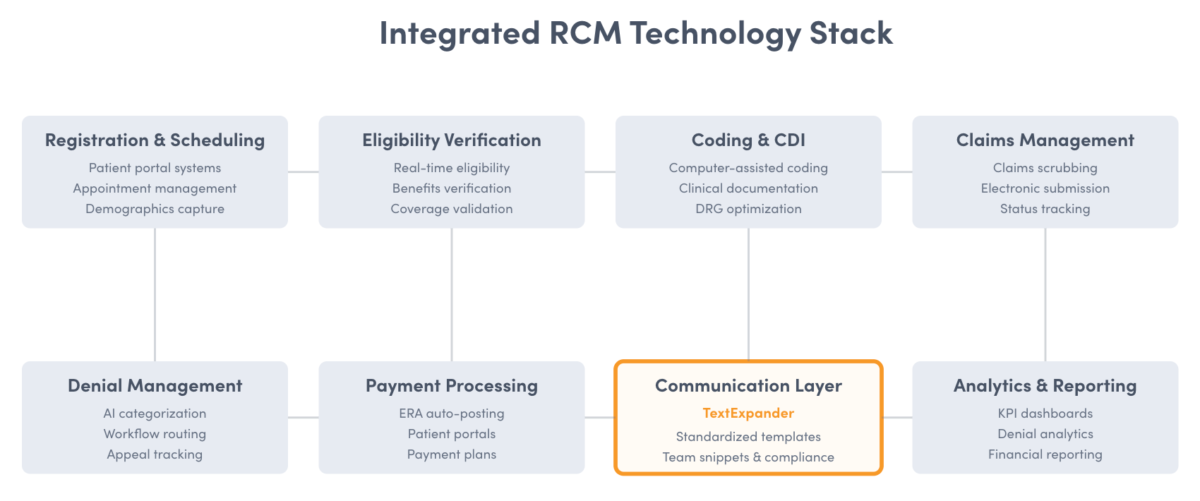
Eligibility verification automation checks coverage in real-time when appointments are scheduled or patients check in. This eliminates manual phone calls to payers and catches coverage issues before services are rendered. Automated verification reduces no-shows from patients who discover coverage issues at check-in and prevents claim denials from outdated insurance information.
Claims scrubbing software identifies errors before submission. Rather than submitting claims to payers where they’ll be denied, scrubbing tools catch issues like invalid code combinations, missing required fields, and authorization number mismatches. This pre-submission quality check improves clean claim rates and reduces time spent on denial rework.
Automated denial management systems categorize denials by reason and route them to appropriate staff for resolution. Rather than having one person manually review all denial notices, automation identifies technical denials that can be quickly corrected, coding denials that need coder review, and medical necessity denials requiring clinical documentation review.
Electronic remittance advice (ERA) auto-posting reduces manual payment entry. When payments arrive electronically with detailed payment information, software can automatically post payments, adjustments, and denials to patient accounts. This speeds up payment posting, reduces data entry errors, and frees staff to work denied claims and patient collections.
Robotic process automation (RPA) handles repetitive, rule-based tasks like checking claim status, downloading remittance advice files, generating standard appeal letters, and updating patient demographics from payer portals. RPA doesn’t replace staff. It eliminates tedious manual tasks so staff can focus on work requiring human judgment.
Artificial intelligence and machine learning predict which claims are likely to be denied before submission. These systems analyze historical denial patterns and flag claims with similar characteristics for review before submission. Early identification of problem claims allows correction before submission rather than denial management after rejection.
Revenue cycle management software integrates multiple functions into unified platforms: patient registration, charge capture, claims submission, payment posting, denial management, and reporting. Integration eliminates duplicate data entry, ensures data consistency across functions, and provides comprehensive visibility into revenue cycle performance.
Patient portal technology improves collections. When patients can view statements online, understand their balances, and make payments electronically, collection rates improve. Portal access also reduces incoming calls from patients checking account status, freeing staff for higher-value work.
Automated appointment reminders reduce no-shows that create revenue loss. Text and email reminders sent 48 hours and 24 hours before appointments give patients time to reschedule if needed. Reduced no-shows mean fewer wasted appointment slots and more revenue captured.
Clinical documentation improvement software helps providers create documentation that supports appropriate coding. These tools suggest documentation elements that might be missing, flag vague terminology that should be more specific, and ensure notes contain required elements for the service level billed.
Technology training requires hands-on practice with actual systems. Don’t just show new staff how software works. Have them complete practice transactions from registration through claim submission and payment posting. Classroom demonstrations don’t build the muscle memory needed for efficient system use.
Ensuring Compliance and Regulatory Adherence
Healthcare billing compliance protects organizations from audits, penalties, and fraud allegations. New staff must understand that billing errors can have legal consequences beyond revenue loss.
HIPAA (Health Insurance Portability and Accountability Act) governs patient information privacy and security. Every RCM staff member handles protected health information (PHI) and must understand disclosure requirements: discussing patient information only with authorized individuals, securing workspaces when stepping away, and using encrypted communication for electronic PHI.
The False Claims Act prohibits submitting claims for services not provided or coded incorrectly. Violations can result in penalties up to three times the amount falsely claimed plus $11,000 per false claim. Train new staff that coding accuracy isn’t just about revenue. It’s about legal compliance. Deliberately billing for services not rendered or upcoding services to increase reimbursement constitutes fraud.
Anti-Kickback Statute prohibits offering or receiving any remuneration in exchange for patient referrals covered by federal healthcare programs. New staff in patient access roles need to understand that providing incentives for patients to choose your practice (beyond normal marketing) can create compliance risk.
Stark Law prohibits physician self-referral for designated health services payable by Medicare or Medicaid. While this primarily affects physicians and ownership structures, billing staff should understand these rules exist to prevent conflicts of interest in medical decision-making.
Medical necessity requirements mandate that services billed must be appropriate for the patient’s condition and supported by documentation. Payers deny services they deem not medically necessary. Train new staff that medical necessity isn’t a billing concept. It’s a clinical standard that billing must reflect accurately.
Modifier usage affects payment and compliance. Modifiers alter code meanings to reflect specific circumstances like bilateral procedures, multiple procedures in the same encounter, or assistant surgeon participation. Incorrect modifier use can trigger claim denials or compliance audits. New staff should learn when modifiers are required and how they affect reimbursement.
Compliance training must include recognizing red flags: pressure to code services not documented, requests to bill for services provided by unlicensed individuals, patterns of upcoding without corresponding documentation changes, and systematic overbilling of any service type. Staff need clear reporting channels for compliance concerns without fear of retaliation.
Regular compliance audits identify problems before they become patterns. Internal audits should review random samples of claims for coding accuracy, documentation support, and proper billing of services provided. When audits reveal issues, immediate retraining prevents continued problems.
Payer contract compliance ensures billing aligns with contracted terms. Each insurance contract specifies allowable billing practices, timely filing requirements, and appeal procedures. New staff should understand that payer contracts supersede general billing rules. What’s allowed for one payer might not be allowed for another.
Updates to regulations happen regularly. The Centers for Medicare & Medicaid Services (CMS) issues annual updates to coding, coverage, and payment policies. Private payers update policies throughout the year. Training must include how staff stay current on regulatory changes that affect billing practices.
See How Affordable Better Compliance Can Be
TextExpander costs just a few hundred dollars annually. Compare that to the $47.77 average cost to rework each denied claim, or the compliance risks of inconsistent documentation.
Financial Reporting and Data Analysis Skills
Revenue cycle reporting converts raw transaction data into actionable insights. New staff need to understand which reports matter and how to interpret them correctly.
Accounts receivable aging reports show outstanding balances grouped by how long they’ve been unpaid: 0-30 days, 31-60 days, 61-90 days, 91-120 days, and over 120 days. Healthy practices keep 70% or more of AR in the 0-30 day category. When aging extends into 90+ days, collection becomes increasingly difficult and write-off risk increases.
Payer mix analysis breaks down revenue by payer type: Medicare, Medicaid, commercial insurance, and patient responsibility. Understanding payer mix helps forecast revenue because different payers reimburse at different rates. Medicare might reimburse 50% of charges while commercial payers reimburse 65%. When payer mix shifts toward lower-reimbursing payers, revenue declines even if patient volume stays constant.
Denial reports should show denial rates by payer, denial reason, procedure code, and provider. This level of detail identifies where problems originate. When one provider has a 20% denial rate while others average 10%, examine that provider’s documentation practices. When one payer denies claims at twice the rate of others, investigate whether you’re meeting that payer’s specific requirements.
Collection reports track how much of billed charges and patient responsibility are actually collected. These reports should separate insurance collections from patient collections because they require different strategies. Insurance collection rates above 95% indicate effective denial management and appeal processes. Patient collection rates above 70% indicate effective patient communication and payment plan offerings.
Productivity reports measure how much work each staff member completes. In RCM, productivity might be measured by: claims processed per day, registration encounters per hour, denial appeals completed per week, or patient accounts resolved per day. Productivity tracking identifies training needs when new staff don’t reach benchmarks and highlights top performers whose techniques can be shared.
Net revenue reports show actual revenue collected after contractual adjustments and write-offs. This differs from gross charges, which represent what was billed. The gap between gross charges and net revenue reveals your effective reimbursement rate. Widening gaps suggest problems with payer contracting, denial management, or bad debt write-offs.
Key performance indicator dashboards consolidate multiple metrics into a single view. Effective dashboards show trends over time, not just current snapshots. When AR days increased from 35 to 45 over three months, that trend indicates a developing problem that requires investigation.
Train new staff to review reports regularly, not just when asked. Weekly review of personal productivity metrics, team denial rates, and AR aging helps staff understand how their daily work impacts overall performance. When someone sees their clean claim rate improving from 88% to 94%, they understand the impact of enhanced accuracy.
Report interpretation requires understanding what numbers mean and why they change. A spike in denials might indicate a payer policy change, new staff making registration errors, or a provider documentation issue. Raw numbers don’t tell you what action to take. That requires investigating the cause behind the change.
Financial forecasting uses historical data to predict future revenue. Understanding seasonal patterns in patient volume, payer mix changes, and denial rate trends helps organizations plan staffing and cash flow. New staff benefit from understanding how their accuracy and productivity affects the organization’s ability to forecast revenue reliably.
Training on Patient-Centric Billing Communication
Patient financial communication directly affects collection rates and satisfaction scores. When patients understand their financial responsibility and feel treated respectfully about billing matters, they’re more likely to pay and return for future care.
Transparency starts at registration. Staff should explain estimated costs before services are provided, verify insurance coverage and patient responsibility, review payment options including payment plans, and confirm patients understand their financial obligation. This upfront conversation prevents surprise bills that damage trust and reduce collection rates.
Patient billing statements must be clear and easy to understand. Avoid medical jargon and insurance terminology in patient-facing documents. Instead of “amount paid by primary payor,” use “amount your insurance paid.” Instead of “patient responsibility after contractual adjustment,” use “amount you owe.” Healthcare communication tools help standardize patient communication so everyone receives the same clear explanation of charges.
Payment plan offerings improve collection rates when patients face large balances. Train staff to proactively offer payment plans before balances age. A patient who agrees to $100 monthly payments is more likely to pay their $1,200 balance than a patient who receives the full balance in a single statement. Payment plans also reduce write-offs by keeping accounts current.
Insurance explanation conversations help patients understand why they owe what they owe. Many patients don’t understand deductibles, coinsurance, or out-of-network charges. When patients receive unexpected bills, they need clear explanations about what services were provided, what insurance paid, why insurance didn’t pay more, and what recourse they have if they believe the charge is incorrect.
Financial assistance programs should be discussed with patients who express inability to pay. Many healthcare organizations offer charity care, sliding fee scales, or prompt pay discounts. Staff need to know what assistance programs exist, eligibility requirements, and application processes. Referring qualified patients to financial assistance improves access to care and reduces bad debt write-offs.
Collection call scripts balance firmness about payment obligations with empathy for financial challenges. Train staff to: confirm the patient’s identity and account details, clearly state the balance owed and payment options available, listen to patient concerns without making promises beyond their authority, and document all collection conversations including commitments made.
Dispute resolution processes address billing errors and patient concerns. When patients question charges, investigate promptly and communicate findings clearly. If the bill was correct, explain why. If an error occurred, correct it immediately and apologize. How organizations handle billing disputes affects patient satisfaction more than the dispute itself.
Digital payment options increase collection convenience. Patients who can pay online through portals, by phone with stored payment methods, or through payment links in emails are more likely to pay promptly than patients who must mail checks. Remove payment friction and collection rates improve.
Bad debt prevention starts with clear communication at registration. When patients understand costs upfront and commit to payment plans early, fewer balances age into bad debt. The cheapest collection dollar is the one collected before the patient leaves the building.
Patient satisfaction with billing processes affects overall satisfaction scores. HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) surveys include questions about billing and financial communication. Patients who felt surprised by bills or treated poorly during collections rate their overall care experience lower, regardless of clinical quality.
Developing Continuous Learning and Role-Specific Training
Revenue cycle management training doesn’t end after initial onboarding. The complexity of healthcare billing, frequent regulatory changes, and payer policy updates require continuous learning.
Role-based training modules customize content to specific positions. Registration staff need deep knowledge of insurance verification but don’t need extensive coding training. Coders need detailed knowledge of documentation requirements but don’t need patient collection training. Billing staff need understanding of claims processing and denial management but don’t need registration protocols. Customize training to the role rather than providing the same content to everyone.
Monthly coding updates keep staff current on changes. ICD-10 and CPT codes change annually in October. New codes are added, old codes are deleted, and descriptions are modified. Create monthly training sessions that review new codes relevant to your specialty, changes to frequently used codes, and updated coding guidelines that affect common procedures.
Payer policy monitoring identifies changes that affect claims processing. Insurance companies update policies throughout the year: authorization requirements for procedures, preferred drug lists, coverage policies for new technologies, and appeal procedures. Assign responsibility for monitoring payer bulletins and create communication processes to ensure staff learn about changes quickly.
Case study reviews use real examples to reinforce concepts. Rather than abstract training on denial management, review actual denied claims from your organization. Walk through what went wrong, how the denial was resolved, and what process changes prevent similar denials. Real examples resonate more than hypothetical scenarios.
Peer learning sessions leverage your top performers’ expertise. Identify staff with consistently high clean claim rates, low denial rates, or strong collection performance. Have them share techniques with colleagues. Peer teaching reinforces learning for both the teacher and learners.
Certification programs demonstrate competency. Professional certifications like Certified Revenue Cycle Specialist (CRCS), Certified Professional Coder (CPC), or Certified Medical Reimbursement Specialist (CMRS) validate knowledge and provide structured learning paths. Support staff pursuing certifications through education reimbursement or time off for exam preparation.
Cross-training builds operational flexibility. When staff understand multiple roles in the revenue cycle, they can provide backup coverage during absences and understand how their work affects downstream processes. A coder who understands claim submission can code more effectively because they know what causes denials.
Knowledge assessments measure learning effectiveness. Pre- and post-training tests show what staff learned, identify persistent knowledge gaps, and verify training effectiveness. When multiple new hires miss the same questions, training needs to better address those concepts.
On-the-job coaching provides real-time feedback during actual work. Rather than discovering errors days later through quality audits, sit with new staff and review work as they complete it. Immediate feedback helps correct technique before bad habits form.
Compliance retraining occurs whenever audits reveal issues. When internal or external audits identify compliance problems, immediate retraining prevents continued violations. Compliance retraining should be documented to demonstrate due diligence if future audits occur.
Measuring Training Effectiveness and Competency
Training investment only matters if it produces measurable improvement. Establish metrics that show whether training achieves intended outcomes.
Pre- and post-training assessments measure knowledge acquisition. Before training begins, test new hires on RCM concepts, coding guidelines, and payer requirements. After training completes, test again using different questions covering the same concepts. Score improvement demonstrates learning effectiveness. Persistently low scores on specific topics indicate training needs enhancement.
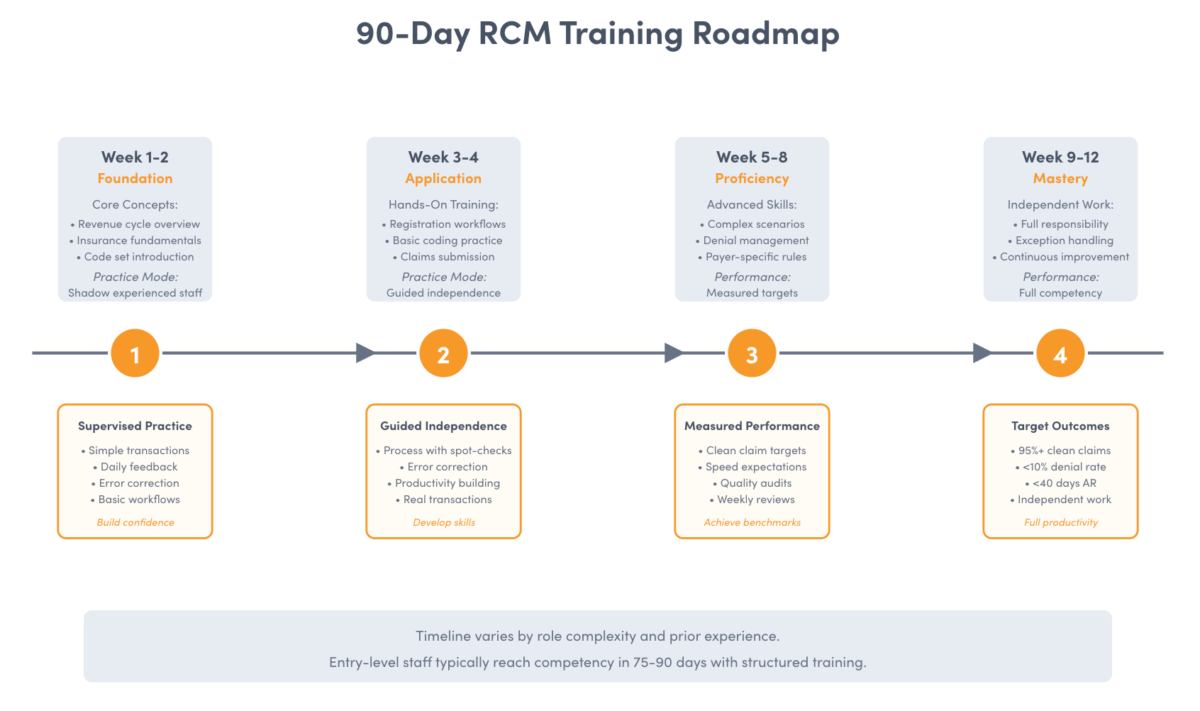
Clean claim rate by staff member shows individual accuracy. Track each staff member’s claims that pass scrubbing and payer acceptance on first submission. New hires should achieve 85% clean claim rates within 60 days and 95% within 90 days. Staff who don’t reach these benchmarks need additional training or may not be suited for the role.
Denial rate by staff member identifies who needs additional coaching. When one person’s claims are denied at twice the rate of colleagues, examine their work for patterns. Are they making registration errors? Coding incorrectly? Billing services without proper authorization? Targeted training addresses specific problems rather than generic refreshers.
Productivity metrics show whether new staff can complete work at acceptable speeds. Measure transactions per hour, claims processed per day, or accounts resolved per week. Productivity increases naturally as new staff gain experience, but staff who don’t reach baseline productivity after reasonable training periods need additional support or different assignments.
Error rate tracking counts mistakes in completed work. Sample completed claims, registration encounters, or payment postings and audit for errors. Calculate error rates as the percentage of transactions containing any error. Target error rates below 5% for critical functions like coding and registration.
Time to competency measures how long new hires need to work independently. Track how many weeks pass before new staff can complete typical transactions without supervisor review. Shorter time to competency indicates effective training and reduces the burden on experienced staff who supervise new hires.
Rework cost quantifies the financial impact of errors. Each denied claim costs $47.77 to rework, according to Premier Inc.’s data. Multiply each staff member’s denials by rework cost to show the financial impact of their accuracy. This concrete number demonstrates why accuracy matters beyond abstract quality standards.
Patient satisfaction scores related to billing measure communication effectiveness. HCAHPS scores include questions about billing communication and financial processes. Track whether patients understood their bills, felt treated respectfully during collection conversations, and received clear explanations of charges. Staff who consistently generate complaints about billing communication need additional training on patient interaction.
Compliance audit findings indicate whether staff follow required procedures. Internal audits should test for proper documentation, accurate coding, appropriate use of modifiers, and timely claim submission. Zero or minimal audit findings demonstrate effective training. Repeated findings on the same issues indicate training gaps.
Retention rates show whether training sets staff up for success. High turnover among new hires often indicates inadequate training that leaves them frustrated and overwhelmed. When new staff stay through their first year, training likely provided the foundation needed for success.
Best Practices for RCM Training Delivery
How you deliver training matters as much as what you teach. Adults learn differently than children, and healthcare professionals need training that respects their time while building practical skills.
Blended learning combines multiple delivery methods: online modules for concepts that don’t require instructor explanation, live sessions for complex topics that benefit from discussion, hands-on practice with real systems and scenarios, and on-the-job coaching that reinforces learning during actual work.
Microlearning breaks complex topics into small chunks delivered over time. Rather than a full-day session on coding, create six 20-minute modules covering specific coding categories. Shorter sessions improve retention and let staff learn without being pulled from work for extended periods.
Just-in-time training provides information when staff need it. Create quick reference guides, cheat sheets, and dot phrase templates that staff access during work. Rather than memorizing payer-specific requirements, staff can look up requirements when processing claims for that payer.
Scenario-based learning uses realistic situations to build problem-solving skills. Present complex registration scenarios where coverage is unclear, coding scenarios where documentation is ambiguous, or denial scenarios requiring appeal strategy. Discussing scenarios as a group builds critical thinking skills that simple rule memorization doesn’t develop.
Spaced repetition improves long-term retention. Rather than teaching a concept once, revisit it at increasing intervals: initial training, review one week later, review one month later, and review three months later. This repetition pattern moves information from short-term to long-term memory.
Gamification increases engagement through friendly competition. Track leaderboards for clean claim rates, create challenges for reducing denial rates, or award points for completing training modules. Recognition and competition motivate some learners more effectively than traditional instruction.
Mentorship programs pair new hires with experienced staff. Mentors provide guidance, answer questions, and help new staff navigate organizational culture and unwritten rules. Effective mentoring accelerates learning and improves retention.
Learning management systems (LMS) organize training content and track completion. LMS platforms deliver online modules, quiz learners on concepts, track which staff completed which training, and identify who needs refresher training. Automated tracking removes administrative burden from training managers.
Video demonstrations show processes that are difficult to explain in text. Record screen captures demonstrating how to navigate billing software, verify insurance eligibility, or review ERA files. Video lets staff watch demonstrations repeatedly until they grasp the process.
Train-the-trainer programs prepare experienced staff to deliver training to others. Your best coders, most accurate registrars, or strongest denial managers may not naturally know how to teach. Provide them with instruction on adult learning principles, presentation skills, and training delivery techniques.
Transform Your RCM Training Program Today
Join healthcare organizations that are reducing claim denials and accelerating new hire productivity with TextExpander. Give your team instant access to standardized templates, payer-specific requirements, and pre-approved messaging that ensures consistency from day one.
The Path Forward: Building Long-Term RCM Excellence
Revenue cycle management training succeeds when it creates staff who understand not just what to do, but why it matters. The difference between a well-trained RCM team and an undertrained one shows up directly on your bottom line: fewer denied claims, faster payment cycles, lower staff turnover, and stronger compliance.
Your training program should evolve as your organization learns what works. Track which training methods produce the best outcomes, identify knowledge gaps that consistently appear, adjust content based on regulatory changes, and incorporate feedback from new hires about what helped most.
The investment in comprehensive training pays for itself through reduced denial rates alone. When 77% of providers report increasing denial rates and each denied claim costs $47.77 to rework, preventing even a small percentage of denials through better training generates substantial ROI.
But the benefits extend beyond immediate financial impact. Well-trained staff experience less stress, feel more confident in their roles, and stay longer with organizations that invest in their development. According to GHR Healthcare, 63% of healthcare organizations face staffing shortages in revenue cycle departments. Effective training helps retain the staff you have.
Start with the fundamentals: make sure new hires understand the revenue cycle’s financial logic, build practical skills through hands-on practice with real scenarios, provide continuous feedback that catches errors early, and measure outcomes so you know training works.
Then expand to advanced topics: payer-specific requirements that affect your organization, technology tools that improve efficiency and accuracy, compliance standards that protect against audits, and analytical skills that turn data into insights.
Your revenue cycle’s effectiveness depends entirely on the people who execute it. Technology can automate tasks and catch errors, but humans make judgment calls, solve complex problems, and build relationships with patients and payers. Invest in those humans through comprehensive training, and the returns compound over years.
Frequently Asked Questions
What is revenue cycle management training?
Revenue cycle management training is the systematic education of healthcare staff on processes from patient registration through final payment collection, including insurance verification, medical coding, claims submission, denial management, and patient billing. Effective training combines foundational knowledge, hands-on practice, and continuous learning to build competent staff who maximize revenue capture while ensuring compliance.
How long should RCM training last for new hires?
Initial RCM training lasts 4-6 weeks depending on role complexity and prior experience. Registration staff often reach competency in 2-3 weeks, while medical coders may need 6-8 weeks. However, training continues beyond initial onboarding through monthly coding updates, payer policy reviews, and ongoing skill development. Plan for new hires to work under supervision for their first 30-60 days before handling work independently.
What are the most critical topics for RCM training?
The most critical RCM training topics include accurate patient registration and insurance verification to prevent claim denials, medical coding fundamentals covering ICD-10, CPT, and HCPCS code sets, claims submission processes and clean claim requirements, denial management strategies and appeal procedures, healthcare compliance including HIPAA and False Claims Act, and patient financial communication techniques that improve collection rates.
How can I measure RCM training effectiveness?
Measure RCM training effectiveness through clean claim rates above 95%, denial rates below 10%, time to competency (weeks until independent work), pre- and post-training assessment scores, error rates in completed work below 5%, and staff retention through first year. Track these metrics by individual staff member and cohort to identify training gaps and continuously improve your program.
Why is ongoing RCM training important?
Ongoing RCM training remains essential because coding sets change annually with new ICD-10 and CPT codes, payer policies update throughout the year affecting authorization requirements and coverage, compliance regulations evolve requiring updated procedures, new technology implementations demand skill development, and staff knowledge degrades without reinforcement. Organizations that invest in continuous learning maintain higher clean claim rates and lower denial rates than those treating training as one-time onboarding.
References
- Experian Health. (2024). State of Claims 2024: Insights from Survey Findings. https://www.experian.com/blogs/healthcare/state-of-claims-2024-insights-from-survey-findings/
- Premier Inc. (2024). Survey of Hospitals, Health Systems and Post-Acute Care Providers. Referenced in: https://www.statnews.com/2024/05/01/insurance-claim-denials-compromise-patient-care-provider-bottom-lines/
- American Hospital Association. (2024). Payer Denial Tactics: How to Confront a $20 Billion Problem. https://www.aha.org/aha-center-health-innovation-market-scan/2024-04-02-payer-denial-tactics-how-confront-20-billion-problem
- The Commonwealth Fund. (2024). Report on Unforeseen Health Care Bills and Coverage Denials by Commercial Insurers. https://www.aha.org/news/headline/2024-08-01-report-highlights-unforeseen-health-care-bills-and-coverage-denials-commercial-insurers
- GHR Healthcare. (2024). Quick Tips for Recruiting and Retaining RCM Professionals. https://www.ghrhealthcare.com/blog/quick-tips-recruiting-and-retaining-rcm-professionals
- Healthcare Innovation Group. (2024). Tips for Training Your Staff on RCM. https://www.hcinnovationgroup.com/finance-revenue-cycle/article/13008187/tips-for-training-your-staff-on-rcm
- DrChrono. (2024). How to Train Staff for Effective Revenue Cycle Management. https://drchrono.com/blog/2024/02/how-to-train-staff-for-effective-revenue-cycle-management/

