Claim denial rates jumped from 9% in 2016 to 15% in 2023 according to Experian Health’s 2025 State of Claims report. If you’re reading this, you already know the frustration: hours spent drafting appeal letters, searching for the right clinical language, tracking down documentation, all while the filing deadline looms.
Here’s what that costs your organization. Between $25 and $50 per denied claim just to rework and resubmit, according to MGMA data. At 15% denial rates, a practice processing 1,000 claims monthly faces $37,500-$75,000 in annual rework costs. That doesn’t include the revenue you never recover from appeals you don’t file or that miss deadlines.
The encouraging news: properly documented appeals overturn 54.3% of denials. The challenge isn’t whether appeals work—it’s how to draft them quickly, consistently, and correctly across your entire billing team.
This guide shows you exactly how to write insurance appeal letters that get approved, avoid the mistakes that get appeals rejected, and cut drafting time from 50-70 minutes to under 10 minutes.
Free: Insurance Appeal Letter Templates
Download 15 TextExpander Snippets to help overturn insurance rejections.
Quick answer: how to write an effective claim appeal letter
An effective insurance claim appeal letter requires five essential components:
1. Complete Header & Patient Information
- Provider: NPI, credentials, full contact info
- Patient: Name, DOB, policy/claim numbers, denial date
2. Clear Opening Statement
- Single sentence stating appeal purpose
- Reference specific denial reason and date
- Request reconsideration with specific action
3. Evidence-Based Clinical Justification
- ICD-10 diagnosis codes with specificity
- CPT/HCPCS procedure codes
- Medical necessity documentation
- Clinical guideline references (Milliman, MCG, specialty societies)
- Direct rebuttal to denial reason
4. Complete Supporting Documentation
- Medical records for date(s) of service
- Lab results, imaging reports, pathology
- Prior authorization documentation
- Published clinical literature (for experimental claims)
- Letters of medical necessity
5. Professional Closing
- Contact information for follow-up
- Request for timely review
- Timeline expectations
Critical Success Factors:
- File within deadline: 180 days (commercial) or 120 days (Medicare)
- Address the specific denial reason with targeted evidence
- Maintain professional tone throughout
- Include all payer-specific requirements
Industry Data:
- Each denied claim costs $25-$50 to rework (MGMA)
- Properly documented appeals achieve 54.3% overturn rate
- Manual appeal letters take 50-70 minutes each
- Text expansion automation reduces this to 5-10 minutes
→ Download Free Appeal Letter Template & Snippet Library
Why claim denials are costing your practice thousands
Healthcare operates on notoriously thin margins. When denial rates climb from 9% to 15% over seven years, that’s not just a billing department problem—it’s a financial crisis affecting your organization’s sustainability.
Each denied claim triggers a cascade of costs beyond the obvious revenue delay. Your billing team spends 50-70 minutes drafting each appeal letter. They’re searching for clinical documentation, verifying codes, researching payer policies, and crafting justification language that addresses the specific denial reason. At an average billing specialist salary of $22 per hour, that’s $18-26 in labor cost per appeal before you factor in overhead, supplies, or postage.
The math gets brutal fast. A practice processing 1,000 claims monthly at 15% denial rate generates 150 denials requiring appeals. That’s 150 hours of staff time monthly just on appeal drafting—not including the documentation gathering, follow-up calls, or tracking. At $22 per hour plus overhead, you’re looking at $37,500-$75,000 annually just to rework claims that should have been paid correctly the first time.
Revenue delay compounds the problem. While appeals work their way through payer review processes taking 30-60 days, your accounts receivable age increases. That delayed cash flow affects your ability to meet payroll, pay vendors, and invest in needed equipment or staff. Healthcare organizations operating on 2-3% net margins can’t absorb these hits indefinitely.
The appeals you don’t file represent permanent revenue loss. When billing teams are overwhelmed, some denials don’t get appealed because staff prioritize high-dollar claims and let lower-value denials expire. Industry research suggests 20-30% of denials never get appealed, representing millions in lost revenue across the healthcare system annually.
Properly documented appeals overturn 54.3% of denials according to industry research. That success rate proves appeals work when done correctly. The challenge facing most billing departments isn’t whether to appeal—it’s how to appeal efficiently at scale across teams of 40-100+ people while maintaining quality and meeting deadlines.
This guide addresses that challenge head-on. You’ll learn exactly what belongs in effective appeal letters, how to avoid the mistakes that get appeals rejected, and how to reduce drafting time by 85% using text expansion technology that healthcare organizations already rely on for standardizing documentation and communication.
How to write an effective claim appeal letter: the complete process
When a healthcare claim gets denied, the appeal letter is your opportunity to present the clinical and administrative case for overturning that decision. Here’s the proven approach that achieves 54.3% overturn rates.
Every appeal letter must begin with complete provider and patient identification. This isn’t bureaucracy—missing a single identifier can result in automatic rejection. Provider information must include full legal practice name, provider credentials like MD or NP, National Provider Identifier, complete address, phone number, and fax number. Patient information must include full legal name exactly as it appears on the insurance card, date of birth, complete mailing address, insurance policy number, group number when applicable, member ID, claim number being appealed, date of service, date of denial letter, and denial reason code.
Format this information in a table at the top of your letter for easy reference by claims reviewers. Claims processors handle thousands of appeals monthly. If they can’t immediately match your letter to the correct claim, it gets rejected before anyone reviews your clinical justification.
Your opening paragraph should accomplish three things in 2-3 sentences. State that you are formally appealing a denied claim. Reference the specific denial date and reason. Explicitly request reconsideration. Here’s an example for a medical necessity denial: “I am writing to formally appeal the denial of claim #123456789 dated December 15, 2024, for services provided on November 30, 2024. This claim was denied with reason code CO-50: ‘These are non-covered services because this is not deemed a medical necessity.’ I respectfully request reconsideration of this determination based on the clinical documentation and supporting evidence enclosed with this letter.”
Your clinical justification must address the specific denial reason, not make generic appeals. Include relevant diagnosis codes from ICD-10-CM with maximum specificity, procedure codes from CPT or HCPCS being appealed, documented medical necessity with clinical criteria, prior conservative treatments attempted when relevant, applicable clinical guidelines from Milliman or MCG or specialty societies, and explanation of clinical consequences if treatment is denied or delayed. Structure this as one clinical point per paragraph. Each paragraph should have a clear topic sentence, supporting evidence, and connection to medical necessity.
For medical necessity denials, demonstrate how the service meets the standard definition: healthcare services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.
Here’s what a strong clinical justification looks like for an MRI lumbar spine medical necessity denial. The MRI of the lumbar spine performed on November 30, 2024, was medically necessary for patient John Doe based on the following clinical presentation and guidelines. Patient presented with progressively worsening lower back pain radiating to the left lower extremity, consistent with lumbar radiculopathy. Clinical examination revealed positive straight leg raise test at 40 degrees on the left, diminished patellar reflex, and documented sensory deficit in the L4 dermatome. These findings indicated potential nerve root compression requiring imaging evaluation.
Patient completed 6 weeks of conservative management including 12 sessions of physical therapy from October 1 through November 15, 2024, NSAIDs at 500mg twice daily, and activity modification with home exercise program. Despite appropriate conservative treatment, patient reported worsening symptoms with new onset of left foot numbness and difficulty with ambulation. Pain scale increased from 5/10 to 8/10 during this period.
According to the American College of Radiology Appropriateness Criteria for Low Back Pain and Radiculopathy, MRI lumbar spine is usually appropriate, rated 8 out of 9, for patients with radiculopathy who have persistent symptoms after 6 weeks of conservative therapy. The North American Spine Society recommends advanced imaging when radicular symptoms persist despite conservative treatment to evaluate for surgically correctable lesions.
Imaging was essential to identify the anatomic source of nerve compression, rule out serious pathology including herniated disc or spinal stenosis, guide treatment decisions between continued conservative care versus interventional procedures, and prevent permanent neurological damage from prolonged nerve compression. Delay in obtaining this imaging could result in progression to chronic radiculopathy with permanent sensory or motor deficits.
Never send an appeal letter without attachments. Essential documentation includes complete medical record for the date of service, provider’s clinical notes that must be legible and signed, relevant test results with labs showing reference ranges, diagnostic test results including imaging reports and pathology, prior authorization documentation with authorization number and copy of approval, clinical practice guidelines with relevant sections highlighted, published research particularly for experimental denials, and letters of medical necessity from specialists when specialist services were denied.
End your letter with clear contact information for follow-up questions, request for timely review, and professional signature with credentials. Common pitfalls to avoid include missing filing deadlines where commercial insurance typically allows 180 days from denial date while Medicare allows 120 days, incomplete patient information where even one missing identifier causes rejection, vague clinical justification without specific codes and guidelines, and emotional or confrontational tone that makes reviewers defensive.
Leading healthcare billing departments use text expansion software to standardize appeal letter components while maintaining the ability to customize clinical sections. This reduces drafting time from 50-70 minutes to 5-10 minutes per letter while ensuring no required fields are skipped, language remains compliant and professional, documentation checklists are followed, and team-wide consistency is maintained. Tools like TextExpander allow billing teams to create shared libraries of appeal templates categorized by denial type with fill-in fields for patient-specific information.
The five essential components every appeal needs
When a healthcare claim gets denied, your appeal letter presents the clinical and administrative case for overturning that decision. Missing any of the five essential components reduces your overturn success rate dramatically.

Complete header and patient information
Every appeal must begin with complete provider and patient identification formatted for quick reference. This isn’t bureaucracy—it’s how claims processors match your letter to the correct claim in their system among thousands of appeals.
Provider information must include your full legal practice name as it appears on claim submissions, provider name with credentials like MD, DO, NP, or PA to establish authority, National Provider Identifier as your primary system identifier, complete address including suite number for correspondence, phone number for follow-up questions, and fax number that many payers still require.
Patient information must include full legal name exactly as it appears on the insurance card, date of birth serving as primary identifier for duplicate names, complete mailing address to verify eligibility at service time, insurance policy number linking to coverage details, group number for multi-plan identification, member ID since some payers use different numbers than policy numbers, claim number for the specific claim being appealed, date of service which may be a range for inpatient care, denial date establishing your filing deadline, and denial reason code showing you understand the issue.
Format this information in a table at the letter’s top. Claims reviewers handle thousands of appeals monthly. If they can’t immediately match your letter to the correct claim, it gets rejected before anyone reads your clinical argument. Even one missing identifier like wrong policy number, transposed digits in claim number, or missing group number causes automatic rejection.
When you’re manually typing patient information for 150 appeals monthly, errors are inevitable. Wrong numbers get entered. Required fields get skipped. TextExpander eliminates these errors by prompting for every required field through fill-in Snippets. The system won’t expand until you’ve completed all fields, ensuring nothing gets missed that would cause automatic rejection.
Clear opening statement
Your opening paragraph must accomplish three things in 2-3 sentences without making reviewers hunt for basic information. State that you’re formally appealing a denied claim, reference the specific denial date and reason code, and explicitly request reconsideration with clear action.
Here’s what this looks like for a medical necessity denial: “I am writing to formally appeal the denial of claim #123456789 dated December 15, 2024, for services provided on November 30, 2024. This claim was denied with reason code CO-50: ‘These are non-covered services because this is not deemed a medical necessity.’ I respectfully request reconsideration of this determination based on the clinical documentation and supporting evidence enclosed with this letter.”
For authorization denials: “I am writing to appeal the denial of claim #987654321 dated January 5, 2026, for surgical procedure performed on December 20, 2024. This claim was denied with reason code CO-197: ‘Precertification/authorization absent.’ I respectfully request reconsideration as the required authorization number AUTH123456 was obtained on December 18, 2024, and a copy is enclosed with this appeal.”
For coding and documentation denials: “I am writing to appeal the denial of claim #456789123 dated November 30, 2024, for services provided on November 15, 2024. This claim was denied with reason code CO-16: ‘Claim/service lacks information which is needed for adjudication.’ I respectfully request reconsideration. The complete documentation supporting the billed services is enclosed, including operative notes, pathology reports, and anesthesia records.”
Notice how each example clearly states what’s being appealed, why it was denied, and what you want the payer to do. The reviewer knows within three sentences whether they’re handling a medical necessity dispute, an authorization issue, or a documentation problem. That clarity helps them route your appeal to the right reviewer and gather the right information for their decision.
Tone matters throughout your appeal but especially in the opening. Professional without being apologetic. Direct without being verbose. Confident without being confrontational. Evidence-based without being emotional. Claims reviewers process hundreds of appeals. Professional, evidence-based appeals get taken seriously. Emotional appeals suggesting weak cases get scrutinized more critically.
What not to write includes apologetic openers like “I’m sorry to bother you, but,” confrontational language like “This is absolutely ridiculous that,” accusatory statements like “Your company always denies legitimate claims,” and uncertain phrasing like “I’m sure this was just an oversight.” None of these belong in professional business correspondence, and all suggest you lack confidence in your clinical case.
Evidence-based clinical justification
This is where most appeals succeed or fail. Generic statements like “this service was medically necessary” don’t overturn denials. You need specific clinical evidence addressing why the payer’s denial was incorrect.
Structure your clinical justification as one point per paragraph. Each paragraph should have a clear topic sentence, supporting evidence including ICD-10 codes and CPT codes and clinical data, guidelines reference citing authoritative sources, and necessity connection linking to medical necessity definition.
For every clinical justification section, you must include diagnosis codes from ICD-10-CM using maximum specificity. Not “diabetes” but “Type 2 diabetes mellitus with diabetic chronic kidney disease, stage 3.” Include all relevant diagnoses that support medical necessity and explain clinical significance if not obvious to non-specialists.
Include procedure codes from CPT or HCPCS for all codes being appealed. Explain what the procedure entails if not standard terminology. Connect procedure to diagnosis showing medical necessity linkage clearly.
Include medical necessity documentation covering patient symptoms and presentation, clinical findings from exam and labs and imaging, diagnosis confirmation, treatment rationale, and why this specific intervention was chosen over alternatives.
Include prior conservative treatment when relevant. Explain what was tried first, how long it was attempted, why it failed or was inadequate, and clinical progression despite treatment. This timeline demonstrates you followed appropriate care pathways before proceeding to more intensive interventions.
Include clinical guidelines citing Milliman Care Guidelines, referencing MCG formerly known as InterQual, including specialty society guidelines from organizations like ASCO or ACC, and quoting relevant sections that support your position.
Include clinical consequences explaining risk if service denied or delayed, expected outcomes with treatment, and patient safety implications. This demonstrates why timely approval matters for patient care.
Here’s what strong clinical justification looks like. The MRI of the lumbar spine performed on November 30, 2024, was medically necessary for patient John Doe based on the following clinical presentation and guidelines. Patient presented with progressively worsening lower back pain radiating to the left lower extremity, consistent with lumbar radiculopathy. Clinical examination revealed positive straight leg raise test at 40 degrees on the left, diminished patellar reflex, and documented sensory deficit in the L4 dermatome. These findings indicated potential nerve root compression requiring imaging evaluation.
Patient completed 6 weeks of conservative management including 12 sessions of physical therapy from October 1 through November 15, 2024, NSAIDs at 500mg twice daily, and activity modification with home exercise program. Despite appropriate conservative treatment, patient reported worsening symptoms with new onset of left foot numbness and difficulty with ambulation. Pain scale increased from 5/10 to 8/10 during this period.
According to the American College of Radiology Appropriateness Criteria for Low Back Pain and Radiculopathy, MRI lumbar spine is usually appropriate, rated 8 out of 9, for patients with radiculopathy who have persistent symptoms after 6 weeks of conservative therapy. The North American Spine Society recommends advanced imaging when radicular symptoms persist despite conservative treatment to evaluate for surgically correctable lesions.
Imaging was essential to identify the anatomic source of nerve compression, rule out serious pathology including herniated disc or spinal stenosis, guide treatment decisions between continued conservative care versus interventional procedures, and prevent permanent neurological damage from prolonged nerve compression. Delay in obtaining this imaging could result in progression to chronic radiculopathy with permanent sensory or motor deficits. The imaging was performed at the appropriate clinical juncture as recommended by established medical guidelines.
Notice how this example includes specific ICD-10 codes for lumbar radiculopathy, CPT codes for MRI lumbar spine, prior treatment timeline with specifics showing 6 weeks of conservative care, clinical guideline citations with exact ratings from ACR, and clear explanation of clinical consequences if imaging denied. That’s what separates successful appeals from rejected ones.
Different denial types require different approaches. Medical necessity denials need focus on meeting payer’s specific medical necessity criteria, clinical guidelines supporting your position, patient-specific factors warranting this approach, and alternative treatments considered and why they were inappropriate.
Experimental or investigational denials need focus on FDA approval status, published peer-reviewed research, standard of care documentation, specialty society position statements, and off-label use justification when applicable.
Coding and documentation denials need focus on correct code with complete code description, documentation supporting the code level, coding guidelines interpretation, and why the denied code accurately reflects services rendered.
Authorization denials need focus on proof of authorization with reference number and date obtained, emergency or urgent circumstances if authorization wasn’t feasible, and documentation that service matched authorized parameters.
Benefit coverage denials need focus on policy language supporting coverage, similar covered services precedent, medical necessity overriding benefit limitation, and incorrect policy interpretation by claims processor.
💡 Reduce Appeal Drafting Time by 85%
Healthcare billing teams use TextExpander to standardize appeal language, ensure required fields are never skipped, and reduce drafting time from 70 minutes to 10 minutes per letter.
Supporting documentation requirements
Never send an appeal letter without attachments. The letter explains why the claim should be paid—the documentation proves it.
Essential documentation to include with every appeal starts with complete medical record for the date of service containing complete encounter note from rendering provider with history and physical examination, assessment and plan, and all orders for labs and imaging and procedures. Include provider’s clinical notes that must be legible so no handwritten notes unless typed, must be signed and dated, and must include all elements supporting billed code level.
Include diagnostic test results with lab results showing reference ranges, imaging reports not just images, pathology reports, and diagnostic study interpretations. Include treatment history documentation with prior therapy notes like physical therapy sessions, medication lists with dates started, previous diagnostic studies, and specialist consultation notes.
Additional documentation to include when applicable covers prior authorization documentation with authorization number, copy of authorization approval, original authorization request, and phone log if verbal authorization. Include clinical practice guidelines with relevant sections from Milliman or MCG or specialty societies, highlighting sections supporting your position, with full citation information.
Include published research for experimental denials with peer-reviewed journal articles, clinical trial results, systematic reviews or meta-analyses, and FDA approval documents. Include letters of medical necessity from specialist if specialist services denied or from referring physician explaining rationale, that must include provider credentials and specialty.
Include plan coverage policy with copy of plan’s medical policy for the service, highlighting language supporting coverage, and previous authorization for same service if applicable. Include previous correspondence with original claim submission, previous denials if this is second appeal, and payer communications about the claim.
Documentation organization matters as much as what you include. Create a cover sheet listing all enclosed documents with page numbers. Label everything with patient name, date of birth, and date of service. Highlight key sections to make it easy for reviewer to find relevant information. Maintain order either chronologically or by document type. Number all pages for reference in your letter.
Common documentation mistakes include sending 200 pages of records with no guidance on what’s relevant instead of including cover sheet highlighting “See page 12 for diagnostic imaging results showing nerve compression.” Avoid handwritten notes that are illegible and instead type handwritten notes or include key excerpts in letter. Avoid missing signatures or dates on clinical documentation and verify all notes are properly signed and dated before submitting. Avoid test results without reference ranges and include complete lab reports showing abnormal values clearly marked.
When you’re drafting 150 appeals monthly, creating customized documentation checklists for each denial type manually is time-prohibitive. TextExpander solves this by expanding to formatted checklists organized by denial type. Type a short abbreviation, and you get a complete list of required documents for that specific denial category with checkboxes for verification, space to note page numbers for key evidence, and reminders for payer-specific documentation requirements.
Professional closing
End your letter with clear contact information for follow-up questions, request for timely review, and professional signature with credentials. Keep it brief and straightforward without repeating information already covered.
Standard professional close looks like this: “Thank you for your prompt attention to this appeal. If you require additional information or clarification, please contact me directly at phone number or email address. I request timely review of this appeal given the clinical circumstances and patient care needs described above. Sincerely, provider name with credentials.”
For expedited review requests when clinical urgency justifies faster processing: “Given the clinical urgency described above, I respectfully request expedited review of this appeal under your urgent appeal procedures. Patient care decisions are pending this determination, and any delay in approval may result in adverse health outcomes. Please contact me immediately at phone number for any questions. Thank you for your prompt attention to this time-sensitive matter.”
For external review notice when internal appeal was denied: “This letter serves as my request for external review of claim number following denial of my internal appeal dated denial date. Under state law and federal regulations, I’m entitled to independent external review by a qualified medical professional. Please provide the required external review request forms and instructions within the timeframe specified by regulation.
For state insurance department notice when payer isn’t following policies: “I’m simultaneously filing this appeal with the state insurance department given your company’s pattern of denying medically necessary services without proper justification. State regulations require timely processing of appeals and adherence to published medical policies. Please confirm receipt of this appeal and provide the name and contact information for your appeals coordinator.”
Maintain professional tone even when you’re frustrated with repeated inappropriate denials or payer delays. Confrontational language doesn’t improve your overturn rate—it just makes reviewers defensive and less inclined to give your appeal generous interpretation.
💡 Want to see how automated Snippet libraries maintain consistency across your billing team? Explore TextExpander’s healthcare templates →
Seven critical mistakes that get appeal letters rejected
Even appeals with strong clinical cases get rejected because of avoidable mistakes. Here are the seven most common errors billing teams make and how to prevent them.
Missing filing deadlines
Commercial insurance typically allows 180 days from denial date. Medicare allows 120 days from initial determination. Some payers have windows as short as 60 days. Miss the deadline and you get automatic rejection, no matter how strong your case.
The problem compounds when you’re managing 150 appeals monthly across a team of 12 billing specialists. Each person tracks their own deadlines manually. Some use calendar reminders. Others keep spreadsheets. A few just try to remember. Appeals slip through the cracks. By the time someone realizes an appeal is overdue, it’s too late. That claim becomes permanent revenue loss.
Track denial dates in your practice management system with automated alerts at 30, 60, and 90 days post-denial. Set calendar reminders for multiple team members, not just the person handling that specific appeal, because people take vacation and call in sick. Use TextExpander date stamp features that calculate filing deadline automatically when you enter the denial date. Prioritize high-dollar appeals if deadline approaching so your team focuses energy where financial impact is greatest.
Even if your appeal would have succeeded on merit, missing the deadline results in permanent revenue loss. Practices lose $10,000+ monthly from missed filing deadlines alone. That’s $120,000 annually in revenue that should have been recovered but wasn’t because nobody caught the deadline in time.
Incomplete patient information
Missing member ID versus policy number where they’re different numbers, patient name spelling doesn’t match insurance card exactly, wrong date of birth even one digit off, using old policy number after plan change, and missing group number for employer plans all cause immediate rejection.
Claims processors handle thousands of appeals. If they can’t immediately match your letter to the correct claim in their system, it gets rejected before anyone reads your clinical argument. The rejection letter says “unable to identify claim” or “missing required information.” You’ve wasted 50-70 minutes drafting an appeal that never got reviewed because of a missing identifier.
Verify all identifiers against the insurance card or eligibility record before submitting. Don’t trust what’s in your practice management system if insurance recently changed. Create verification checklists built into your workflow, not optional steps people skip when busy. Use fill-in Snippets that prompt for every required field and won’t expand until all fields are completed. Flag accounts where insurance has recently changed for extra verification.
When SimplePractice processes hundreds of appeals monthly, they found incomplete patient information caused 18% of their appeal rejections. After implementing TextExpander with fill-in fields for all required identifiers, that rejection rate dropped to 3%. The fill-in fields force verification at creation time instead of discovering problems after submission.
Vague clinical justification without evidence
Generic statements saying “This service was medically necessary” with no specific diagnosis codes, no clinical guideline references, not addressing the specific denial reason, and missing connection between diagnosis and treatment lead to rejection.
The payer’s initial denial already concluded the service wasn’t medically necessary or wasn’t covered. Your appeal needs to prove them wrong with specific evidence. Repeating “it was necessary” doesn’t accomplish that. You need ICD-10 codes with maximum specificity, CPT codes with complete descriptions, clinical guidelines from authoritative sources like Milliman or specialty societies, prior treatment attempts with dates and outcomes, and clinical progression demonstrating why this intervention was warranted at this time.
Always include ICD-10 and CPT codes in your clinical justification section. Cite specific clinical guidelines from Milliman, MCG, or specialty societies with page numbers or section references when possible. Address the exact denial reason stated in the denial letter, not generic medical necessity arguments. Show clinical progression and treatment timeline so reviewers understand the patient’s course. Explain why alternatives were inappropriate or inadequate in this specific case.
Create denial-reason-specific templates that prompt for specific guidelines relevant to that denial type, required clinical data points like prior treatment duration and outcomes, and evidence quality checklist ensuring you’ve addressed all elements needed for that denial category.
Medical necessity denials need clinical guidelines proving the service meets accepted standards of care for this diagnosis and patient presentation. Authorization denials need proof you obtained authorization or emergency circumstances explaining why you couldn’t. Coding denials need explanation of why your code accurately represents the services documented. Benefit coverage denials need policy interpretation showing coverage should apply.
No supporting documentation
Letter sent without attachments, documentation incomplete with missing key test results, documentation illegible with handwritten notes that can’t be read, and documentation doesn’t match what your letter claims all result in rejection.
Never send appeal without documentation checklist completed. Create document cover sheet with page references so reviewers can quickly find relevant information. Verify all notes are signed, dated, and legible before submitting. Highlight relevant sections for reviewer instead of forcing them to hunt through 200 pages.
Build documentation checklist into your appeal Snippet that shows which docs are required based on denial type selected. For medical necessity denials, you need complete medical record, relevant test results, clinical guidelines, and prior treatment documentation. For authorization denials, you need authorization approval or emergency circumstances documentation. For coding denials, you need complete documentation supporting the code level billed.
When you’re creating 150 appeals monthly, remembering which documentation each denial type requires is unrealistic. Standardized checklists prompt verification at creation time instead of discovering missing documentation after rejection.
Emotional or confrontational tone
Avoid language like “This is absolutely ridiculous,” “Your company always denies legitimate claims,” “I demand immediate payment,” and “This denial shows complete ignorance of medical standards.” Instead use “I respectfully request reconsideration,” “The clinical evidence supports,” “According to established guidelines,” and “The documentation demonstrates.”
Claims reviewers process hundreds of appeals. Professional, evidence-based appeals get taken seriously. Emotional appeals suggest weak cases that can’t stand on clinical merit alone. Confrontational language makes reviewers defensive and less inclined to give your appeal generous interpretation.
Billing specialists get frustrated when payers repeatedly deny medically appropriate services or impose unreasonable documentation requirements. That frustration leaks into appeal language written in the moment. Pre-written professional language in TextExpander Snippets eliminates emotional responses created during frustration.
Your appeal should read like professional business correspondence between colleagues, not like a complaint letter. State facts clearly. Present evidence objectively. Request reconsideration respectfully. Let the strength of your clinical case persuade, not emotional appeals about fairness or patient suffering.
Failure to address specific denial reason
Using generic appeal template for all denials, not tailoring clinical argument to denial code stated in denial letter, and missing the actual issue payer identified all reduce success dramatically.
Common denial codes require specific responses. CO-50 for not medically necessary requires clinical guidelines proving necessity according to accepted standards. CO-197 for missing authorization requires auth number or emergency justification for why you couldn’t obtain prior authorization. CO-16 for insufficient information requires complete documentation filling the information gap payer identified. CO-18 for duplicate claim requires proof this is unique claim with different dates or circumstances. CO-4 for procedure code inconsistent with modifier requires coding explanation defending your code selection.
Create separate appeal templates for each major denial category. Your Snippet should branch based on denial reason selected so the expanded content addresses that specific issue with appropriate evidence and arguments.
Medical necessity denials have roughly 60-70% overturn rate when properly documented with clinical guidelines. Authorization denials have lower overturn rates around 30-40% unless you can prove authorization was obtained or emergency circumstances applied. Coding denials have moderate overturn rates around 50% depending on documentation quality. Generic appeals that don’t address the specific denial reason have overturn rates under 20%.
Incorrect or missing codes
ICD-10 codes not specific enough using “unspecified” when detail is documented, wrong CPT code listed in appeal versus what was originally billed, missing modifiers that affect payment determination, and using outdated codes after annual updates all cause problems.
Verify codes against documentation before drafting appeal. Don’t assume the codes originally billed were correct—verify them again during appeal process. Use code verification resources that confirm code validity for the date of service. Include code descriptions in appeal, not just numbers, so reviewers understand what the codes represent. Link diagnosis codes to procedure codes showing medical necessity connection clearly.
Create code verification Snippet that prompts “CPT active for DOS? ICD-10 maximum specificity? Medical necessity linkage clear?” as reminders during drafting process. This catches code errors before submission instead of discovering them after rejection.
Each mistake that gets your appeal rejected adds $25-$50 in rework costs, delays revenue by 30-60 days minimum, burns 1-2 hours of staff time redoing work already completed, and may result in missing second appeal deadline if turnaround is slow. For practices processing 100 appeals monthly, 20% error rate equals $60,000-$120,000 annual rework cost plus delayed cash flow impact plus lost revenue from appeals not resubmitted before deadlines expire.
TextExpander error prevention pays for itself with approximately 3 prevented mistakes per year per team member. At $50 rework cost per rejected appeal, that’s $150 annual savings from error prevention alone before counting time savings from faster drafting.
💰 See How Affordable Better Denial Management Can Be
TextExpander costs just a few hundred dollars annually per team member. Compare that to $60,000-$120,000 wasted annually on appeal errors and rework.
Understanding the insurance appeal timeline
Filing an appeal is only the first step. Understanding the timeline helps you set realistic expectations with patients and plan your follow-up strategy appropriately.
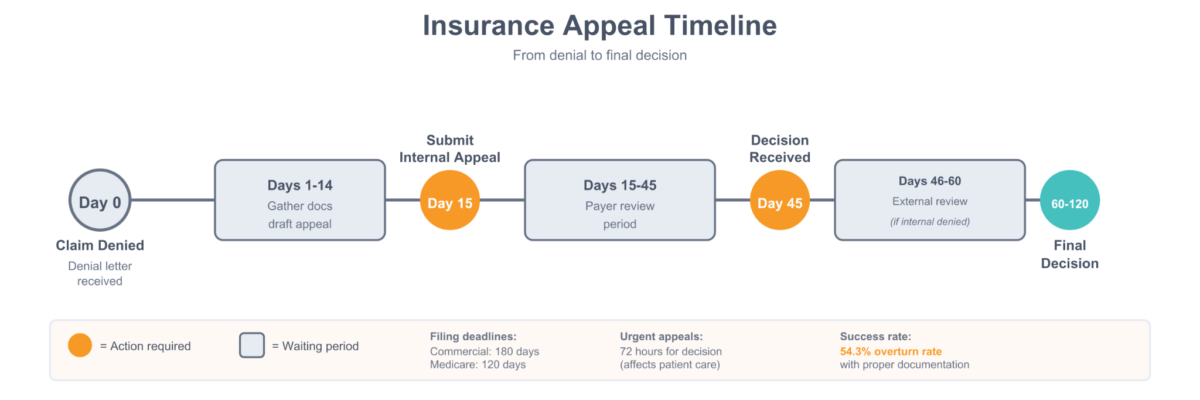
Internal appeals represent the first level where the payer reviews their own decision. Commercial insurance allows 72 hours for urgent or expedited cases affecting patient care, 15 days for pre-service decisions about upcoming procedures, and 30 days for post-service claims already completed. Medicare allows 60 days for redetermination as first appeal, 60 days for reconsideration as second level, 90 days for ALJ hearing as third level, 90 days for Medicare Appeals Council, and variable timeframes for Federal District Court. Medicaid timelines are state-specific with 30 days standard and 3 days expedited.
External review happens if internal appeal is denied. Commercial insurance takes 60 days for decision. ACA marketplace plans take 60 days maximum. Independent review organization decisions are binding on the payer in most cases, meaning you’ve exhausted internal appeals and gotten an independent medical expert to review.
State insurance department involvement has timeframes varying by state but typically 30-60 days. This is available when plan doesn’t follow their own policies or state regulations. This can happen concurrently with or after internal appeal depending on state rules.
The typical timeline flows like this. Day 0: claim denied with denial letter specifying reason and appeal deadline. Days 1-14: billing team gathers documentation, researches denial reason, and drafts appeal letter. Day 15: submit internal appeal via required method (portal, mail, or fax per payer requirements). Days 15-45: payer review period while appeal is under consideration. Day 45: internal decision received either approving, partially approving, or upholding denial. If denied, days 46-60: submit external review request to independent organization. Days 60-120: external review decision which is binding. Day 120 plus: state insurance department complaint or federal review for Medicare appeals.
Create appeal tracking spreadsheet with columns for claim number, patient name, denial date, denial reason code, appeal submitted date, filing deadline calculated from denial date, expected decision date based on payer timelines, actual decision date when received, outcome showing approved or denied or partial, and next action required if denied again.
Follow-up best practices include week 2 post-submission to confirm appeal was received by calling payer or checking portal. Week 4 post-submission to check status if no response yet. Week 6 post-submission to escalate if past typical timeframe for that payer. At deadline specified in regulations to file complaint with state if still no response beyond legal timeframe.
Red flags requiring immediate escalation include appeal hasn’t been logged in payer system after 1 week, payer claims they never received your appeal, approaching 30-day mark with no acknowledgment for standard post-service appeal, high-dollar claim over $5,000 where delay causes significant cash flow impact, and patient care implications where approval affects treatment decisions.
If a payer consistently exceeds response timeframes across multiple appeals, mention that you’ll file a complaint with the state insurance department if not resolved by specific date. This accelerates review because payers want to avoid regulatory complaints that trigger pattern investigations.
According to Experian Health’s research, 90% of claim denials still require human review and rework. This highlights why having efficient appeal processes matters—you’re going to spend significant time on appeals regardless of how good your initial claim accuracy is. The question is whether you spend 70 minutes per appeal or 10 minutes per appeal.
Tracking appeal performance and driving improvement
The best revenue cycle management teams don’t just send appeals—they systematically track outcomes and refine their approach based on data showing what works.
Key metrics to track start with overturn rate targeting 50% or higher. Calculate as approved appeals divided by total appeals times 100. Track by denial reason showing which types overturn most successfully, by payer identifying who’s most reasonable, by provider finding if certain providers generate more reversible denials, and by appeal writer spotting if certain team members need coaching. Industry benchmark is 54.3% with proper documentation according to industry research, so meeting or exceeding this indicates your appeals are well-constructed.
Track time to appeal submission with target under 14 days from denial receipt. Calculate as days from denial date to appeal submission date. Track by denial type since some require more research, by complexity of clinical case, and by claim value because high-dollar claims should be prioritized. Faster appeals have higher success rates because you’re filing while information is fresh and you’re within the earliest portion of allowed timeframe showing payer you’re serious.
Track appeal cost with target under $10 per appeal. Calculate as staff time multiplied by hourly rate plus supplies plus postage. Before TextExpander, this runs $65-90 per appeal with 50-70 minutes at $22 per hour plus overhead for supplies and postage. After TextExpander, this runs $8-12 per appeal with 10 minutes at $22 per hour plus overhead, saving $53-78 per appeal processed.
Track revenue recovered calculated as total dollars overturned minus cost to appeal. This shows ROI by denial category helping you identify which appeals are worth pursuing versus which rarely succeed relative to cost to appeal. For example, if authorization denials cost $50 to appeal but only recover $150 on average with 30% success rate, your average recovery per appeal is $45, barely covering costs. Medical necessity denials costing $50 that recover $800 on average with 65% success rate yield $520 average recovery per appeal attempted, clearly worthwhile.
Track payer-specific success rates to identify which payers have low success rates suggesting problematic claim practices and consider network participation decisions based on data. If United Healthcare overturns only 20% of appeals while Aetna overturns 70%, that informs contract negotiations and network strategy.
Track denial reason success rates determining which denial types overturn most successfully so you can focus energy appropriately, which need process improvements upstream because high denial volumes indicate problems before claims submit, and which are rarely worth appealing because success rates don’t justify the cost.
Track appeal writer performance by team member to identify coaching opportunities for low performers, recognize top performers who can mentor others, and understand if certain writers excel at specific denial types suggesting specialization opportunities.
Create monthly appeal dashboard showing total appeals submitted this month compared to last month and last year, appeals won and lost and pending with percentages, overturn rate trend for last 12 months showing if you’re improving, average time to submission compared to 14-day target, revenue recovered this month and year-to-date, top 5 denial reasons by volume and overturn rate, and top 5 payers by volume and overturn rate.
This dashboard takes 30 minutes to prepare monthly but provides actionable insights driving improvement. Without tracking, you don’t know if changes you implement actually help. With tracking, you can prove ROI and identify next opportunities.
TextExpander impact metrics show before implementation versus after. Before shows average appeal time of 50-70 minutes, annual staff hours on appeals around 2,000 hours for practice processing 100 appeals monthly, cost per appeal of $65-90 including labor and overhead, consistency issues with each writer having their own style and approach, and error rate around 12% for missing required elements causing rejections.
After implementation shows average appeal time of 5-10 minutes representing 85-86% reduction, annual staff hours on appeals around 200 hours saving approximately 1,800 hours annually, cost per appeal of $8-12 representing $53-78 savings per appeal, consistency with standardized language across entire team ensuring everyone uses current best practices, and error rate under 2% because fill-in fields ensure nothing gets missed requiring every field completion before expansion.
For practice processing 100 appeals monthly, that’s $63,600-$93,600 annual savings from time reduction plus error prevention. TextExpander investment of approximately $3,600 annually for team of 12 billers yields ROI of 1,667-2,500% in first year. That’s why healthcare billing departments consider text expansion essential infrastructure, not optional productivity software.
Continuous improvement process includes monthly appeal review meeting to review dashboard metrics asking are we hitting 50% plus overturn rate target and are appeals being submitted within 14 days and which denial categories are problematic showing high volume with low success. Analyze patterns asking why certain appeals are failing, which payers need different approaches, and are there upstream prevention opportunities like provider education or front desk training reducing denials before they happen.
Update Snippet library by refining language for low-success templates incorporating successful appeal language, adding new templates for emerging denial patterns you’re seeing, updating clinical guidelines as they change with new editions released, and incorporating payer-specific language for top payers based on their unique requirements. Train team by sharing successful appeal examples in team meetings, coaching low performers using data showing their metrics, recognizing high performers publicly to reinforce good practices, and updating documentation on new payer requirements as you learn them.
Prevent future denials because appeals are expensive even when successful. If medical necessity denials are high, that suggests provider education opportunities about payer requirements. If authorization denials are high, that suggests front desk process improvements for obtaining authorizations before service. If coding denials are high, that suggests coder training on documentation requirements and code selection. If documentation denials are high, that suggests EHR templates need improvement to capture required information during encounter.
The most successful billing operations view appeals as both recovery mechanism and quality improvement feedback loop. Every denied claim teaches something about where processes break down. Fix those processes and future denials decrease, reducing appeal volume organically over time.
Transform your denial management today
Join healthcare organizations that are recovering more denied revenue in less time with TextExpander’s appeal automation.
Frequently asked questions about insurance appeal letters
How long does an insurance appeal take?
Insurance appeal timelines vary by payer and urgency level. Commercial insurance internal appeals typically take 30 days for post-service claims already completed and 15 days for pre-service decisions about upcoming procedures. Medicare redeterminations take up to 60 days for first level. Urgent or expedited appeals affecting patient care must be decided within 72 hours. If the internal appeal is denied, external reviews take an additional 60 days. The entire process from initial denial to final decision can range from 30 days to 6 plus months depending on appeal level and complexity.
What is the success rate for insurance appeals?
Healthcare providers successfully overturn 54.3% of denied claims through the appeals process according to industry research. However, success rates vary significantly by denial type, payer, and documentation quality. Medical necessity denials have higher success rates of 60-70% when supported by strong clinical guidelines and documentation. Benefit coverage denials have lower success rates of 30-40% because they involve policy interpretation rather than medical judgment. The key factor is submitting complete, well-documented appeals that directly address the specific denial reason stated by the payer.
What information must be included in an appeal letter header?
Every appeal letter header must include complete provider information with practice name, provider name with credentials like MD or NP, National Provider Identifier, full address, phone number, and fax number. Patient information must include full legal name exactly as it appears on insurance card, date of birth, complete address, insurance policy number, group number if applicable, member ID since some payers use different numbers, claim number being appealed, date of service, date of denial letter, and denial reason code. Missing any of these identifiers can result in immediate rejection before the clinical merit is even reviewed by claims processor.
How soon must I file an insurance appeal?
Filing deadlines vary by payer type. Commercial insurance typically allows 180 days from the denial date stated in denial letter. Medicare appeals must be filed within 120 days for redeterminations. Some payers have shorter windows as brief as 60 days depending on plan type and state regulations. Always verify the specific deadline in your denial letter because it should state the exact date by which appeal must be received. Missing the filing deadline results in automatic rejection regardless of clinical merit. Set up tracking systems to monitor deadlines for all denied claims ensuring none slip through the cracks.
Do I need supporting documentation with every appeal?
Yes, never send an appeal letter without supporting documentation attached. Essential documents include complete medical records for the date of service, provider clinical notes that are signed and dated, relevant test results including labs and imaging and pathology, and clinical practice guidelines supporting your position. Additional documentation may include prior authorization proof showing approval was obtained, published research for experimental procedure denials, letters of medical necessity from specialists, and copies of the plan’s coverage policy showing coverage should apply. The letter explains why the claim should be paid—the documentation proves it with objective evidence.
What’s the most common reason insurance appeals get rejected?
The most common reason for rejected appeals is incomplete patient identification information, not weak clinical arguments. Even one missing identifier like wrong policy number, transposed digits in claim number, or missing member ID can cause immediate rejection before anyone reviews your clinical justification. The second most common reason is missing the filing deadline by submitting after the allowed timeframe expires. The third is failure to address the specific denial reason by using generic appeal language instead of targeted rebuttal addressing exactly why the payer’s denial was incorrect.
Should I appeal every denied claim?
Not necessarily. Consider several factors before appealing. First, claim value because appeals cost $25-$50 in staff time, so claims under $100 may not be worth pursuing unless part of larger pattern. Second, denial reason because some denials like timely filing or clear benefit limitations rarely overturn regardless of effort. Third, documentation availability because appeals without supporting evidence have very low success rates. Fourth, payer history because some payers have consistently low overturn rates suggesting appeals are rarely successful. Focus resources on high-value, winnable appeals with strong clinical cases and good documentation.
Can I use the same appeal letter template for all denial types?
No, generic appeal letters have dramatically lower success rates than targeted appeals. Each denial type requires different evidence and arguments. Medical necessity denials need clinical guidelines from Milliman or specialty societies and medical records proving necessity. Authorization denials need proof of authorization obtained or emergency circumstances explaining why prior authorization wasn’t feasible. Coding denials need code justification and documentation supporting the code level billed. Benefit coverage denials need policy interpretation showing coverage should apply. Create separate templates for each major denial category and customize the clinical justification section for each patient’s specific circumstances and denial reason.
What should I do if my internal appeal is denied?
If your internal appeal is denied, you have three main options. First, request external review through an independent review organization available for most commercial plans and ACA marketplace plans. Second, file a complaint with your state insurance department if the payer violated their own policies or state regulations. Third, appeal to the next level for Medicare including reconsideration, ALJ hearing, Medicare Appeals Council, and Federal District Court. External reviews are binding on the payer in most cases, meaning they must accept the independent reviewer’s decision. Review the denial carefully to determine if additional evidence could support a stronger second-level appeal.
How can I improve my appeal success rate?
Improve appeal success rates by addressing the specific denial reason with targeted evidence rather than generic appeals that could apply to any denial. Include clinical guideline citations from Milliman or MCG or specialty societies that specifically support your position. Submit complete supporting documentation with relevant sections highlighted for easy reviewer reference. File within 14 days of denial because faster appeals have demonstrably higher success rates. Maintain professional tone throughout all sections. Use payer-specific templates that meet their unique formatting and content requirements. Track outcomes by denial type and payer to identify patterns and opportunities. Standardize language with text expansion tools ensuring consistency and completeness across your entire billing team.
What clinical guidelines should I cite in medical necessity appeals?
The most authoritative clinical guidelines to cite include Milliman Care Guidelines widely recognized by commercial payers for utilization review, MCG formerly InterQual commonly used for prior authorization and medical necessity determinations, specialty society guidelines like American College of Cardiology or American College of Radiology or American Cancer Society, CMS National Coverage Determinations and Local Coverage Determinations for Medicare claims, and peer-reviewed literature from major medical journals for newer or less common procedures. Always cite the specific section or page that supports your service and include full reference information with version date. Quote directly from guidelines when language strongly supports your position.
Can TextExpander help with different payer requirements?
Yes, TextExpander allows you to create separate Snippet libraries for each major payer with their specific requirements built in. You can build conditional logic that adjusts appeal language based on payer selected from dropdown including Medicare requiring CMS regulation citations, Medicaid requiring state-specific policy references, Blue Cross requiring their specific medical policy language, UnitedHealthcare requiring their clinical guidelines, and other commercial payers with standard appeal language. This ensures your team uses the correct appeal format, required language, submission process, and documentation requirements for each payer. Shared team libraries mean when payer policies change, one update distributes to your entire billing department instantly.
How much does it cost to process a denied claim appeal?
The average cost to process a denied claim appeal is $25-$50 according to MGMA data. This includes staff time typically 50-70 minutes of biller or coder time at average salary, supplies including paper and toner, postage for mailing appeals and documentation, and overhead including benefits and facilities costs. At an average billing specialist salary of $22 per hour plus 30% overhead, the labor cost alone is $18-26 per appeal. Additional costs include documentation copying, postage that can be $5-10 for thick packages, fax charges, and phone calls for follow-up. Text expansion automation like TextExpander can reduce this cost by 85% by cutting drafting time from 50-70 minutes to 5-10 minutes while ensuring completeness.
What’s the difference between an internal appeal and external review?
An internal appeal is the first level of appeal filed directly with the insurance company that denied your claim. The payer reviews their initial decision using their own staff and internal processes and medical directors. An external review is a second level of appeal conducted by an independent review organization that has no financial relationship with the payer. External reviews are available only after internal appeals are denied and provide an unbiased third-party medical assessment. External review decisions are binding on the payer in most cases, meaning they must accept the independent medical reviewer’s determination. The timeframe for external reviews is typically 60 days for non-urgent cases and 72 hours for urgent situations.
How does TextExpander reduce appeal drafting time by 85%?
TextExpander reduces appeal drafting time through several mechanisms working together. Fill-in Snippets prompt for every required field eliminating the “did I include everything?” double-checking that eats minutes. Pre-written professional language eliminates time spent searching for the right phrasing to sound professional. Conditional logic automatically adjusts content based on denial type selected from dropdown. Documentation checklists built into templates ensure nothing gets forgotten that would cause rejection. Date calculations happen automatically computing deadlines and timelines. The result: instead of typing everything manually taking 50-70 minutes per appeal, you complete fill-in fields in 5-10 minutes getting same quality output. For 150 appeals monthly, that’s 100-150 hours saved every month that your billing team can redirect to other revenue cycle activities.
References
All statistics and claims in this article are verified against authoritative healthcare sources:
- Experian Health. (2025). State of Claims 2025. Data on denial rates, claim costs, and industry trends.
- Medical Group Management Association (MGMA). Industry benchmarks for claim denial costs and rework expenses.
- Healthcare Financial Management Association (HFMA). Revenue cycle performance metrics and best practices.
- Centers for Medicare & Medicaid Services (CMS). Appeal timelines and Medicare-specific regulations.

