Love working with patients, hate having to manually enter data to create medical progress notes? You’re not alone.
Unfortunately, there’s no getting around creating these standard medical records. Medical progress notes are important for monitoring the efficacy of treatments and communicating patient information. They’re also essential for the filing of health insurance reimbursement claims.
While you can’t do away with medical progress notes completely, you can complete them more quickly using TextExpander.
Write medical progress notes faster with TextExpander
TextExpander is a shorthand typing tool that lets you summon up words, phrases, and templates with minimum typing.
Using TextExpander, you can create templates for medical progress notes and make them appear on any page or platform with just a couple of keystrokes.
TextExpander’s customization features enable you to create flexible templates. You can add form fields, checkboxes, and dropdown lists to make them even easier to fill out.
TextExpander also functions as a knowledge repository for storing repetitive codes, terms, and phrases. You can create a library of standard medical terms, phrases, and descriptors on TextExpander to add them to documents without having to fully type them.
You can also share them with your team to ensure that everyone uses the correct terminology and appropriate language when recording patient care and treatment.
Dr. Jeremy Sharp, aka The Testing Psychologist, uses TextExpander to insert diagnostic codes, write results sections, populate recommendations, and sign reports in seconds. He created a series of helpful videos to illustrate how he does this — we encourage you to check them out!
“Every keystroke saved, is time saved, which means I can do my job longer and see more children.” — Dr. Melanie Hsu
Try TextExpander TodayWrite medical progress notes faster
Here are essential tips for writing clinical patient notes more quickly.

Use templates
SOAP, BIP, DAP, PIRP, BIRP. No matter what type of medical progress note you use, there’s a template for it.
And that’s a good thing. Templates save you time and eliminate the need for creating records from scratch.
Electronic health record (EHR) software programs usually offer template options. However, if you do not have EHR software, you can download templates online. Alternatively, you can design your own template based on your unique needs.
Use a ready-made template or design your own; just don’t waste time creating medical progress notes from scratch.
Use checkboxes and dropdown lists
When creating your own medical progress note template, or adapting an existing one, be sure to add checkboxes, dropdown menus, and similar features whenever possible.
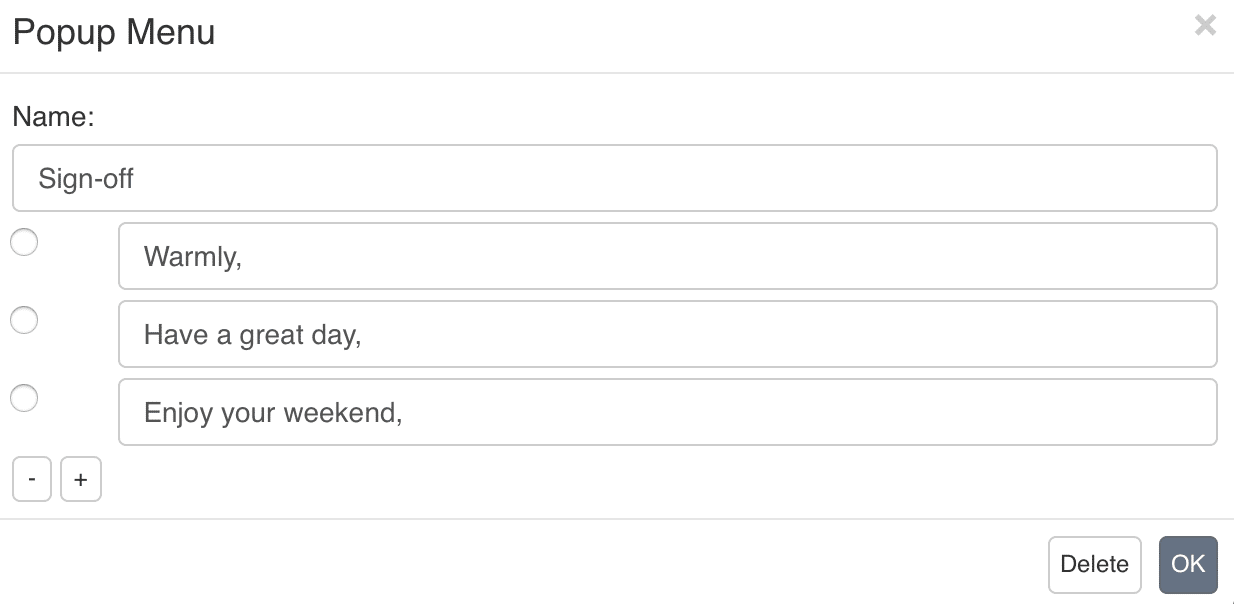
Having lists of items to select, as opposed to just fill-in-the-blanks form fields, saves you time since it reduces the amount of searching and typing that you need to do.
Lists and menus also have the advantage of preventing spelling errors and freeing you from having to rely on memory to add specific, hard-to-remember information.
Save standard terms, phrases, and descriptors
Instead of typing standard terms, phrases, and descriptors from scratch each time, type them only once and save them somewhere accessible for the next time you need to use them.
The idea is to create a library of standard phrasing and vocabulary — including intervention words, patient presentation descriptions, themes of sessions, treatment approaches, diagnostic codes, and more — so you can add them to your clinical patient notes without having to fully type them.
If you don’t have software that provides this already, you can create your own lists of frequently-used terms and phrases. Some of these lists are available online — this list of commonly used intervention words for mental health progress notes is an example.
“Progress notes planner”-style books such as this one also provide a comprehensive catalog of health-related terms and descriptions for different types of practices.
Having a repository of essential phrases to draw from when creating medical notes isn’t just a time-saving measure — it’s also a way to ensure you use the right spelling as well as the correct tone and language every time.
Try TextExpander free for 30 days
TextExpander saves medical practitioners, therapists, veterinarians, dentists, and other health care professionals hours each month by eliminating the need to fully type repetitive words, codes, and phrases.
Incorporating TextExpander into your workflow will not only help you create medical progress notes faster but will save you time that you can use to focus on work that really matters to you.
Related Resources
- Best Practices for TextExpander and HIPAA / Medical / Personal Info
- Best Patient Follow Up Email Templates to Use in 2023
- Getting Started With TextExpander
FAQ about medical progress notes
How can I speed up my medical documentation?
Take advantage of templates, checklists, and drop-down menus, and save standard terms, phrases, and descriptors in a text-expansion tool.
How long should it take to write a progress note?
The time it takes to write a medical progress note can vary widely based on several factors:
- Complexity of the Case: A straightforward, routine follow-up might require a brief note, while a complex case with multiple issues could necessitate a more detailed note.
- Purpose of the Note: A note written for a routine outpatient visit might be shorter than one written for an inpatient with multiple daily changes in condition or treatment.
- Experience of the Provider: More experienced providers might be able to write notes more quickly due to familiarity with common conditions and treatments, as well as proficiency in medical documentation.
- Electronic Medical Record (EMR) System: Some EMR systems have templates or auto-populate features that can speed up the documentation process, while others might be more cumbersome and time-consuming. They can be enhanced with third-party software like TextExpander.
- Institutional or Departmental Requirements: Some medical institutions or departments have specific guidelines or requirements for documentation that can influence the length and detail of a progress note.
- Personal Style: Some providers prefer to write detailed notes to ensure comprehensive documentation, while others might be more concise.
On average, for a routine follow-up or uncomplicated case, it might take anywhere from 5 to 15 minutes to write a progress note. For more complex cases, especially in an inpatient setting, it could take 20 minutes or longer. However, it’s essential to prioritize the quality and accuracy of the note over speed. Proper documentation ensures continuity of care, provides a legal record, and can play a crucial role in patient outcomes.
Can you reduce charting time?
Yes, reducing charting time is possible without compromising the quality and accuracy of medical documentation. Here are some strategies to streamline the charting process:
- Use Templates: Many Electronic Medical Record (EMR) systems offer customizable templates for common conditions or visit types. By using these templates, providers can quickly document routine information, making modifications as needed for individual patients.
- Voice Recognition Software: Consider using voice recognition software that transcribes spoken words into written text. This can be especially helpful for providers who can dictate faster than they can type.
- Standardized Phrases or Macros: Create a list of standardized phrases or macros for commonly used sentences or paragraphs. A tool like TextExpander can help with this, and it can significantly speed up the documentation process.
- Auto-Populate Features: U the auto-populate or auto-fill features in EMRs, which can automatically pull in relevant data from other parts of the patient’s chart.
- Stay Organized: Keep a consistent order when documenting, such as always charting systems in the same sequence. This can help establish a rhythm and reduce the time spent searching for information.
- Chart in Real-Time: Whenever possible, document during the patient encounter. This can help reduce the need to recall details later and can save time in the long run.
- Delegate Appropriately: For tasks that don’t require a physician’s expertise, such as entering vital signs or updating medication lists, delegate to nurses or medical assistants when appropriate.
- Limit Interruptions: Try to minimize interruptions while charting. This might mean setting specific times for documentation or finding a quiet place away from high-traffic areas.
- Continuous Training: Stay updated with any new features or updates in the EMR system. Regular training can introduce time-saving features or shortcuts that providers might not be aware of.
- Feedback and Review: Periodically review your charting process and seek feedback from colleagues. They might have tips or tricks that you haven’t considered.
- Use Mobile Devices: Some EMR systems have mobile apps that allow providers to chart on-the-go, which can be especially useful during rounds or in between patient visits.
- Stay Concise: While thorough documentation is essential, avoid unnecessary verbosity. Be clear and concise, providing all the necessary details without redundancy.
Remember, while the goal is to reduce charting time, it’s crucial to maintain the accuracy, clarity, and comprehensiveness of medical records. Proper documentation is vital for patient care, communication among healthcare providers, and legal protection.
What can progress notes include in a medical record?
Progress notes in a medical record provide a chronological account of the patient’s clinical status, treatment, and response to care. They play a crucial role in ensuring continuity of care, facilitating communication among healthcare providers, and serving as a legal record of the care provided. Here’s what progress notes can typically include:
- Patient Identification:
- Full name
- Date of birth
- Medical record number or other identifiers
- Date and Time: The date and time of the encounter or when the note was written.
- Subjective Data:
- Chief complaint or reason for the visit/hospitalization
- History of present illness (HPI)
- Review of systems (ROS)
- Any other relevant patient-reported information
- Objective Data:
- Vital signs (e.g., blood pressure, heart rate, temperature, respiratory rate)
- Physical examination findings
- Results of diagnostic tests or imaging studies
- Assessment:
- Diagnosis or differential diagnoses
- Summary of the patient’s current clinical status
- Plan:
- Diagnostic tests or procedures to be ordered
- Treatment recommendations, including medications, therapies, or surgeries
- Patient education or counseling provided
- Follow-up or referral plans
- Medications:
- Any new medications prescribed, including dosage, route, and frequency
- Changes to existing medications
- Notation of any medication refills
- Patient’s Response to Treatment:
- Improvement or worsening of symptoms
- Any side effects or adverse reactions to treatments
- Interactions and Coordination of Care:
- Consultations with or referrals to other specialists
- Discussions with family members or caregivers
- Patient’s Understanding and Concerns:
- Questions the patient may have asked
- Any concerns or hesitations regarding the treatment plan
- Future Care Planning:
- Anticipated changes in treatment or care
- Goals for future visits or treatments
- Provider Identification:
- Name and title of the healthcare provider writing the note
- Signature or electronic authentication
- Additional Information (if relevant):
- Informed consent discussions
- Risk factors or barriers to care
- Social or environmental factors impacting health
Progress notes should be clear, concise, and accurate, reflecting the clinical thought process and decision-making of the healthcare provider. They should be written in a timely manner to ensure the most accurate documentation of the patient’s care.
What is the difference between progress notes and medical records?
Progress notes and medical records are essential to documenting patient care, but they serve different functions and encompass different aspects of a patient’s healthcare journey. Here’s a breakdown of the differences:
- Definition:
- Progress Notes: These are specific entries made by healthcare providers that detail the clinical status, treatment, and care plans for a patient during a particular encounter or over a period of time. They provide a chronological account of the patient’s condition and response to treatment.
- Medical Records: This is a comprehensive collection of all the documentation related to a patient’s health, care, and treatments over time. It includes progress notes but also encompasses many other types of documentation.
- Scope:
- Progress Notes: Typically focus on specific encounters or periods of care, such as a particular clinic visit, hospital day, or therapy session.
- Medical Records: Include a wide range of documents, such as admission and discharge summaries, surgical reports, diagnostic test results, imaging studies, medication lists, immunization records, and more.
- Purpose:
- Progress Notes: To provide a detailed account of a patient’s condition, treatment, and progress during specific encounters. They ensure continuity of care by informing other healthcare providers about what has been done and what the plan is moving forward.
- Medical Records: To provide a comprehensive and holistic view of a patient’s health history and care over time. They serve as a repository of all health-related information for a patient, ensuring that any provider can understand the patient’s health background and previous care.
- Contributors:
- Progress Notes: Typically written by the healthcare provider directly involved in the patient’s care during a specific encounter, such as physicians, nurses, therapists, or other clinicians.
- Medical Records: Include contributions from a wide range of healthcare professionals, administrative staff, and sometimes even patients (e.g., through patient portals).
- Duration:
- Progress Notes: Reflect care and observations for specific, often shorter, periods.
- Medical Records: Span the entirety of a patient’s life or the duration they have been seen within a particular healthcare system or facility.
- Confidentiality:
- Both progress notes and medical records are confidential and are protected by laws and regulations, such as the Health Insurance Portability and Accountability Act (HIPAA) in the U.S. Access to this information is restricted to authorized individuals.
In summary, while progress notes are individual entries that detail specific encounters or periods of care, medical records are the comprehensive collection of all health-related documentation for a patient. Both are crucial for ensuring high-quality patient care, informed decision-making, and legal documentation.
What not to include in patient notes?
When documenting patient care, it’s essential to maintain professionalism, accuracy, and respect for patient privacy. Here are some things that should not be included in patient notes:
- Subjective or Judgmental Language: Avoid using language that could be perceived as biased, derogatory, or judgmental. Stick to objective and factual descriptions.
- Irrelevant Personal Information: Do not include details about a patient’s personal life, relationships, or other information that is not directly relevant to their medical care.
- Speculation: Stick to the facts. Avoid including unconfirmed hypotheses or speculations about a patient’s condition or behavior.
- Redundant Information: Avoid repetitive documentation that doesn’t add value to the patient’s record.
- Abbreviations That Aren’t Standard: While many medical abbreviations are universally recognized, avoid using abbreviations that could be ambiguous or misunderstood.
- Identifiable Third Parties: Do not include names or other identifying information about third parties (e.g., family members, friends) unless it’s clinically relevant and with appropriate consent.
- Informal Language or Slang: Maintain a professional tone and use medical terminology appropriately.
- Protected Health Information (PHI) Without Consent: This includes photographs, videos, or other media of the patient without their explicit consent.
- Personal Opinions or Feelings: Keep personal emotions or opinions about the patient, their family, or their situation out of the medical record.
- Financial Information: Avoid including specific financial details, such as insurance policy numbers or payment information, unless it’s in the appropriate section of the medical record designed for that purpose.
- Unsecured or Unprotected Information: Any information that could compromise the patient’s privacy or the security of their data should not be included.
- Placeholder or Incomplete Notes: Avoid leaving placeholder notes or incomplete entries that might be forgotten or overlooked later.
- Copy-Pasting Without Verification: While electronic health records (EHRs) allow for copying and pasting, it’s essential to verify the information to ensure its accuracy and relevance to the current note.
- Offensive or Inappropriate Content: This includes any content that could be considered disrespectful, discriminatory, or inappropriate in a professional setting.
- Information Covered Elsewhere: Avoid duplicating information that’s already documented in another part of the medical record, unless it’s necessary for clarity or emphasis.
Always prioritize the patient’s privacy, rights, and best interests when documenting care. Ensure that notes are clear, accurate, and provide a comprehensive picture of the patient’s health and care while avoiding unnecessary or inappropriate content.

